
How to eat bread, rice, and potatoes without blood sugar spikes

What if I told you that cutting out bread, rice, and potatoes completely — the very foods that form the heart of countless cuisines — isn’t just unrealistic, but unnecessary? For many of us, these foods aren’t just calories; they’re comfort, family, and culture. Yet, when diagnosed with diabetes or insulin resistance, people are often told to banish them forever. That kind of advice can feel like a lifetime sentence to bland, joyless meals.
The truth is, you don’t have to give them up. You can absolutely eat carbohydrates — including your favorite starches — without sending your blood sugar on a dangerous roller coaster. The key is learning to work with your body’s biology instead of against it.
In this article, I’ll walk you through practical, science-backed strategies that can help flatten your post-meal glucose spikes, improve your insulin sensitivity, and make your meals both satisfying and metabolically friendly. These are not restrictive diet rules — they’re smart adjustments to how and when you eat.
By the end, you’ll know how to transform your starches in your own kitchen, the ideal order to eat your meals, and why even a short post-dinner walk can be as powerful as medication. And as always, this information is for educational purposes — talk to your physician before making major changes to your diet or medication.
Key Takeaways
-
Transform Your Starches: Cooling and reheating starchy foods like rice and potatoes increases resistant starch, which reduces glucose spikes.
-
Never Eat Carbs Naked: Always pair carbohydrates with protein, fat, or acid to slow sugar absorption.
-
Sequence Your Meals: Eat vegetables and protein first, and carbs last, to dramatically lower post-meal glucose.
-
Walk It Off: A 10-minute walk after eating helps muscles pull glucose from your bloodstream.
-
Choose Logs, Not Kindling: Whole, high-fiber carbs release energy slowly, unlike processed “fast-burning” carbs.
-
Mind the Clock: Avoid eating late at night — your body handles sugar best earlier in the day.
1. Harness the Power of Resistant Starch
If you love rice, potatoes, or pasta, you’re in luck. One of the most underrated tools in blood sugar management is resistant starch — a form of starch that behaves more like fiber than sugar.
Normally, starches are quickly broken down into glucose, flooding your bloodstream with sugar. But resistant starch “resists” digestion. It passes through your small intestine largely intact, ending up in your large intestine where it becomes food for your gut bacteria.
This fermentation process creates beneficial short-chain fatty acids like butyrate, which has powerful metabolic effects. Butyrate improves insulin sensitivity, reduces inflammation, strengthens your gut lining, and even supports brain health.
Here’s the simple kitchen trick:
-
Cook your starchy food — say, rice or potatoes.
-
Let it cool completely in the refrigerator for 12–24 hours.
-
Reheat it before eating.
This “cook-cool-reheat” cycle triggers starch retrogradation, a process that changes part of the starch structure into resistant starch. Studies show that cooled and reheated rice or potatoes can reduce post-meal glucose spikes by up to 30–40% compared to freshly cooked versions.
Other naturally rich sources of resistant starch include beans, lentils, peas, oats, and barley. Think of these as your gut-friendly, glucose-stabilizing allies.
2. Master the Art of Food Pairing
If you’ve ever heard the phrase “never eat a naked carb,” take it seriously. What you eat with your carbohydrates can make or break your blood sugar response.
Carbs eaten alone digest quickly, but adding protein or healthy fat slows everything down. For example, pairing rice with chicken or tofu, or spreading avocado on toast, dramatically blunts the glucose curve.
Research backs this up: a meta-analysis of over 150 studies found that adding protein to a carbohydrate meal can cut glucose spikes in half. That’s a massive difference for such a simple change.
Fat also helps. Healthy fats — like olive oil, avocado, nuts, and seeds — delay gastric emptying, meaning glucose enters your bloodstream more gradually. This is why adding olive oil to pasta or butter to potatoes produces a steadier energy release.
And then there’s acid — a hidden gem for blood sugar control. Vinegar, lemon juice, or fermented foods like sauerkraut can reduce the rate at which starches break down into glucose. In fact, a tablespoon of vinegar before or during a meal has been shown to improve insulin sensitivity by 20–30%.
So, dress your meals smartly: a squeeze of lemon, a splash of vinaigrette, or a side of pickles can do wonders.
3. Change Your Meal Order: Eat Carbs Last
This might be the simplest, most surprising strategy of all: the order you eat your food matters.
If you start your meal with bread or juice, your blood sugar will spike sharply. But if you eat your vegetables and protein first, you create a “nutrient shield” that slows digestion.
Imagine coating your stomach with fiber and protein before adding carbs — this literally slows the absorption of glucose. The result? A smaller, gentler glucose curve instead of a steep mountain peak.
A well-known study in people with type 2 diabetes found that eating vegetables and protein before carbohydrates led to a 40% lower glucose spike and a 31% reduction in insulin levels compared to eating carbs first.
When dining out, resist the breadbasket at the start. Wait for your salad or main dish, and enjoy your carbs after. It’s a small behavioral change with big metabolic benefits.
4. Take a Walk After You Eat
You don’t need fancy gym sessions to improve your blood sugar — just move your body after meals.
Even a 10-minute stroll after eating can lower post-meal glucose significantly. Why? Because your muscles act as glucose sponges. When you walk, especially using your soleus muscles in your calves, your body immediately starts burning glucose for energy, pulling it from your bloodstream.
This isn’t just theory — studies show that light movement after meals can lower blood sugar as effectively as some glucose-lowering medications. The key is timing: move within 30 minutes after eating, even if it’s just cleaning up, walking around your home, or climbing stairs.
It’s simple, free, and incredibly effective.
5. Choose Your Carbs Wisely: Logs, Not Kindling
Let’s clear up a common misconception: carbs aren’t the enemy — refined carbs are.
Imagine your metabolism as a campfire. Processed carbs like white bread, pastries, or sugary snacks are like kindling — they ignite instantly, burn hot, and die fast, leaving you hungry and drained.
Whole carbs, on the other hand, are logs — slow, steady, and sustainable. Foods like steel-cut oats, quinoa, lentils, beans, and brown rice release glucose gradually, providing consistent energy.
The secret weapon here is fiber. Fiber slows sugar absorption, supports gut health, and increases satiety — helping you feel full longer. Aiming for 25–35 grams of fiber daily can make a dramatic difference in glucose stability.
So don’t cut out carbs — upgrade them. Swap white rice for brown or basmati, replace white bread with whole grain, and choose lentil or chickpea pasta instead of refined flour versions.
6. Respect Your Body Clock: Don’t Eat Late
Your metabolism follows a circadian rhythm, meaning your body processes food differently throughout the day. Insulin sensitivity peaks in the morning and declines by night.
When you eat late — especially carb-heavy meals — your body struggles to clear glucose effectively. Add melatonin (your sleep hormone) into the mix, which further suppresses insulin release, and you have a recipe for overnight hyperglycemia.
In simple terms: your body is designed to digest during the day and repair at night.
To work with your biology, aim to eat your last meal at least three hours before bedtime. This gives your system time to digest, stabilize glucose, and prepare for restorative sleep.
If you’re used to late dinners, start by shifting mealtimes 30 minutes earlier each week. Even small changes can significantly improve fasting glucose levels and next-day energy.
Conclusion: Carbs Aren’t the Enemy — Knowledge Is Power
Living with diabetes or insulin resistance doesn’t mean saying goodbye to the foods you love. It means learning to enjoy them intelligently.
By applying these six simple, science-backed strategies —
-
Boosting resistant starch,
-
Pairing your carbs with protein, fat, or acid,
-
Eating carbs last,
-
Walking after meals,
-
Choosing high-fiber “log” carbs, and
-
Respecting your body’s natural rhythm —
—you can dramatically flatten your blood sugar curve and support your body’s healing process.
These habits don’t just protect your glucose levels — they enhance energy, improve digestion, and support long-term heart and metabolic health.
You don’t need to fear bread, rice, or potatoes. You just need to understand them. With the right knowledge, you can take control of your metabolism and enjoy food with freedom and confidence again.
Your plate can be both delicious and diabetes-friendly — all it takes is knowing how to eat smarter, not stricter.
News in the same category

What really happens to your body when you take LOSARTAN

Stop Eating Eggs Immediately If Your Body Shows These 8 Signs
Sarcopenia: Causes of Muscle Loss and How to Regain Strength

Yarrow: A Timeless Herbal Ally with Amazing Health Benefits
How To Use a Frozen Lemon To Fight Malignant Tumors in The Body
Top 11 Nutrients To Destroy Cancer Stem Cells

Cocoa flavanols may protect blood vessels even when you sit for hours
Major Signs You Are Magnesium Deficient (and What To Do About It!)

30 Anti-inflammatory Foods That Block Inflammation & Joint Pain (backed by science)

2 Signs of Kidney Failure: If Your Morning Urine Shows This Sign, See a Doctor Immediately

If You’re Not Using Castor Oil You’re Missing Out

Silent heart attack — the pain no one recognizes in time
The HIDDEN cause of neck and shoulder pain nobody talks about

Health officials issue warning over ‘very contagious’ disease spreading across US state

🫁 1 Cup to Cleanse Your Lungs of Phlegm and Toxins Naturally

🦷 The #1 Best Remedy for Dental Plaque and Tartar Buildup (Dentist-Approved Home Method)
10 Proven Ways to Lower Uric Acid Naturally (Backed by Science)
News Post

Eat more, weigh less? 5 surprising ways foods can help you burn fat
What really happens to your body when you take LOSARTAN

Stop Eating Eggs Immediately If Your Body Shows These 8 Signs
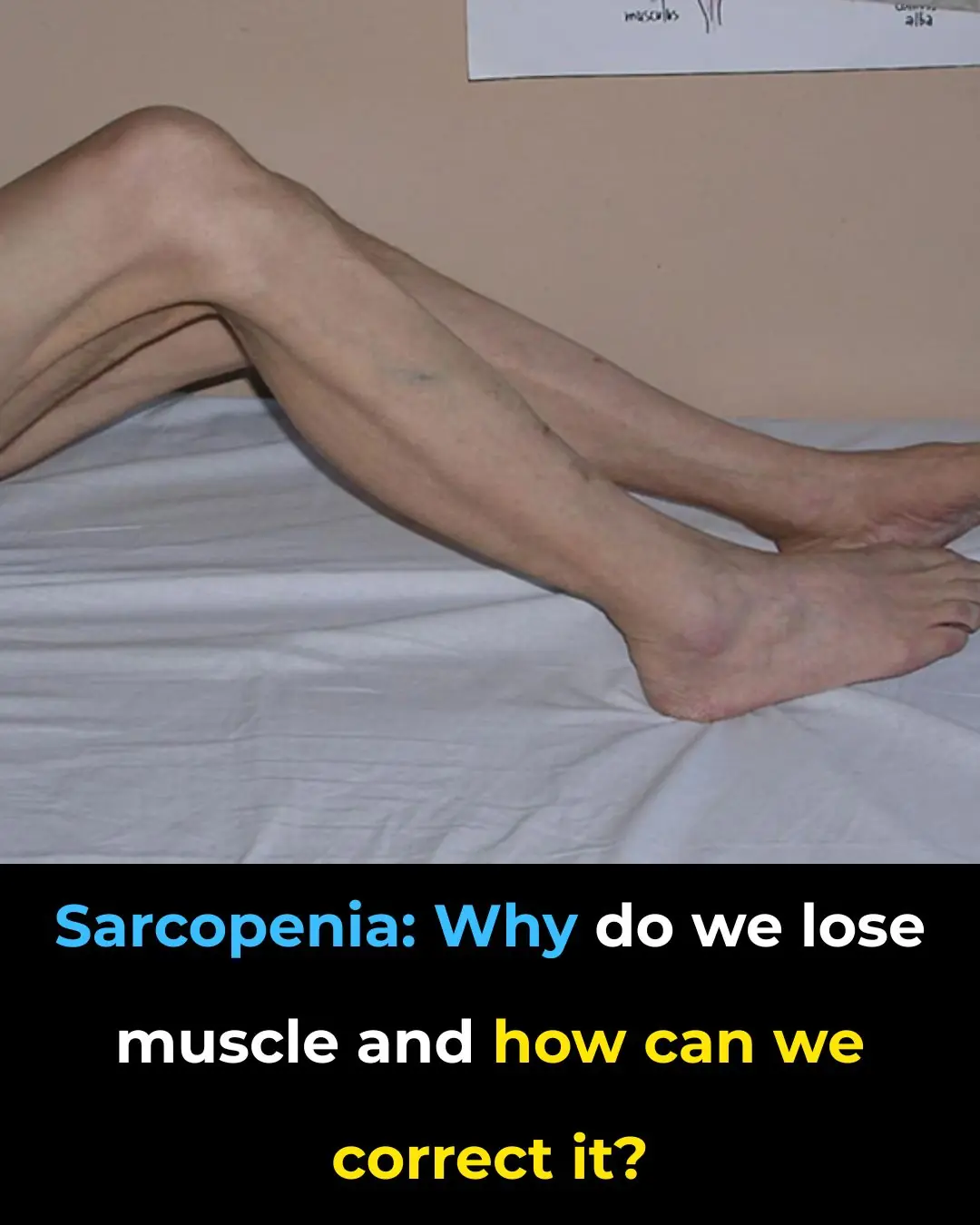
Sarcopenia: Causes of Muscle Loss and How to Regain Strength

Yarrow: A Timeless Herbal Ally with Amazing Health Benefits

The Heartbeat of Compassion: The Unlikely Hero Who Saved a Hippo's Life

Zoo in Thailand Shut Down After Bears in Giant Hamster Balls Turn on Guests

A Pitcher’s Second Chance: How a High School Classmate Stepped Up to Save Steven Register’s Life

Rooting for Will: A Tuesday of Joy Before a Wednesday of Courage

Two Hearts That Needed Each Other.

The Mother Who Delivered More Than Food.

The Boy Who Paid for a Stranger’s Meal When No One Was Watching.
How To Use a Frozen Lemon To Fight Malignant Tumors in The Body

Can I Eat Without Hiding Now?

He Thought It Was Just Another Shift — Until a Life Was Placed in His Hands.

How to make fragrant and nutritious passion fruit peel jam
The refrigerator gasket is moldy, use this to clean it, it will be clean in just 5 minutes

How to make spicy and sour pickled cabbage to eat during Tet

Winter drink lemon honey ginger water, body 5 special benefits
