
Risk Of Prostate Cancer Increases By 45% In Men Who Share This Common Practice
Recent research has revealed a shocking and alarming trend: men who neglect one essential health habit may be putting themselves at a significantly higher risk of developing prostate cancer. This newfound understanding has grabbed the attention of medical professionals, who are now emphasizing the importance of this issue, as early intervention could be a matter of life and death.
The American Cancer Society points out that about one in eight men will face a prostate cancer diagnosis at some point in their lives. Currently, prostate cancer is the second leading cause of cancer-related deaths among men, second only to lung cancer. Though approximately one in 44 men will ultimately succumb to this disease, many individuals who are diagnosed early go on to live long, healthy lives. The key factor that separates these survivors from others is often the timeliness of their diagnosis and treatment.
One crucial health practice that men tend to overlook is regular prostate cancer screenings. Skipping these screenings can raise the risk of dying from prostate cancer by as much as 45%. Despite being a simple and relatively quick procedure, many men either ignore or delay this step, and this decision could have severe consequences.
National guidelines, including those for prostate-specific antigen (PSA) testing, offer a potentially life-saving opportunity. PSA tests, which are typically conducted via a blood test, can detect prostate cancer in its earliest stages, giving doctors a vital window of time to initiate treatment. Research supporting the benefits of early detection is substantial and compelling, with mounting evidence showing that PSA screenings significantly improve survival rates.
One of the most influential studies in this area is the European Randomized Study of Screening for Prostate Cancer (ERSPC), which has collected data over the past two decades. This landmark study involved participants from seven European countries and included tens of thousands of men. The findings have been consistent and clear: regular screenings can reduce the risk of dying from prostate cancer by up to 20%.
Despite this overwhelming evidence, a troubling trend is emerging: fewer men are attending their scheduled screenings. This drop in participation correlates with an increase in deaths from prostate cancer. The difference in mortality between those who attend regular screenings and those who do not is stark and alarming.
A comprehensive study led by scientists from the Erasmus MC Cancer Institute at the University Medical Centre in the Netherlands examined 72,460 men and found significant discrepancies in outcomes based on screening participation. Around one in six men missed every scheduled screening, and these non-attenders had a 45% higher risk of dying from prostate cancer compared to their peers who participated in screenings.
On the other hand, those who adhered to regular screenings saw a 23% reduction in their risk of dying from prostate cancer. This data highlights the clear benefit of proactive health engagement. Experts speculate that men who avoid screenings may also be avoiding other important healthcare practices, which in turn leads to worse outcomes.
Dr. Renée Leenen, the lead researcher and a prominent figure at the Erasmus MC Cancer Institute, has suggested that men who skip these screenings may be exhibiting a broader tendency of neglecting preventive healthcare. These men might be "care avoiders," people who avoid medical care altogether, even when it's in their best interest. In contrast, men who make a habit of attending screenings often exhibit healthier lifestyles, which may include better nutrition, exercise, and a general focus on health maintenance.
Understanding why certain men choose not to engage in preventive care is critical for healthcare professionals. By uncovering the reasons behind these decisions, public health programs could be tailored more effectively to encourage broader participation in prostate cancer screenings. Ultimately, increasing attendance at these screenings is a major step toward improving the success of national prostate cancer screening initiatives.
This research will be presented at the upcoming European Association of Urology (EAU) Congress in Madrid, Spain. The goal of this presentation is to raise awareness of these issues and to inspire tangible changes in healthcare practices, both in Europe and globally.
For men, the message is straightforward yet crucial: regular prostate cancer screenings can save lives. When caught early, prostate cancer is much more treatable and manageable. The consequences of ignoring these screenings, however, can be devastating.
Interestingly, the link between health habits and cancer outcomes extends beyond just screening attendance. Men who maintain healthier lifestyles, such as eating well, exercising regularly, and managing stress, are more likely to attend screenings. This reflects the idea that good health practices often go hand in hand, creating a powerful cycle of health and prevention.
Reluctance to visit a doctor for screenings may stem from a variety of reasons, including fear, denial, or simply the busyness of life. Unfortunately, these factors can lead to preventable outcomes. Health professionals are urged not only to offer convenient and accessible screening options but also to prioritize education about the importance of early detection. Awareness campaigns that stress the life-saving potential of prostate cancer screenings could significantly increase participation rates.
Programs aimed at reducing barriers to screening could revolutionize prostate cancer outcomes. Providing flexible scheduling, conducting outreach in communities with low screening rates, and crafting messages that resonate with at-risk populations could all play a pivotal role in improving overall screening participation.
PSA testing, which was once the subject of skepticism due to concerns over overdiagnosis and overtreatment, has evolved significantly. Recent improvements in screening technologies and follow-up care have helped to address these issues, making the test more reliable and accurate. Modern PSA testing protocols aim to strike a balance between the benefits of early cancer detection and the risks of overdiagnosing cancers that may never progress.
Alongside PSA testing, other diagnostic tools have been developed, including MRI scans and prostate biopsies, which provide additional layers of diagnostic accuracy. Together, these tools significantly improve the likelihood of catching cancers that need treatment while avoiding unnecessary interventions for slow-growing tumors that pose little threat.
The psychological benefits of screening should not be underestimated. Men who regularly attend screenings often report greater peace of mind, knowing that they are actively monitoring their health. Furthermore, a consistent relationship with healthcare providers fosters trust, creating an environment in which men feel comfortable addressing concerns and asking questions.
For men who remain hesitant about PSA testing, healthcare professionals recommend initiating open and honest discussions. Talking about family history, lifestyle choices, and personal risk factors can help men make more informed decisions about their health and wellness.
While prostate cancer can be a serious diagnosis, it is not necessarily a death sentence. Many forms of prostate cancer grow slowly and can be managed successfully if detected early. Available treatment options, such as surgery, radiation, hormone therapy, and active surveillance, are most effective when administered in the early stages of the disease. By staying vigilant and proactive, men can significantly improve their chances of successful treatment and recovery.
The financial burden associated with treating late-stage prostate cancer is staggering. In contrast, early detection often leads to simpler, less invasive treatments that require fewer resources and result in better long-term outcomes. On a broader scale, widespread participation in national screening programs could save healthcare systems billions of dollars while also saving lives.
Family members play a vital role in encouraging men to take their health seriously. A strong support system can make a huge difference in health outcomes, and loved ones can help motivate men to attend regular screenings. Communities, too, have an important part to play in fostering a culture of health awareness. Local health campaigns, community outreach programs, and public education efforts can increase awareness and participation in prostate cancer screenings.
In conclusion, experts agree that regular prostate cancer screenings are not merely a recommendation — they are essential for saving lives. The risks of avoiding these appointments are simply too great. Men are encouraged to take charge of their health, make time for screenings, and remain proactive in managing their well-being.
Healthcare systems should focus on making screenings more accessible and eliminating the barriers that prevent men from attending. Education, outreach, and compassion can drive significant improvements in prostate cancer survival rates. As the findings from this important study are shared with the world, it is hoped that more men will take the crucial first step toward early detection and treatment. Prostate cancer can be managed — but only if men prioritize early diagnosis.
News in the same category

Chewing Gum Releases Microplastics Into Saliva – Even Natural Gums Are Not Safe, Study Finds
STUDY SHOWS SWITCHING TO PERSONAL CARE PRODUCTS WITHOUT CERTIAN PRESERVATIVES TURNS BREAST CANCER GENES OFF IN 28 DAYS
Study finds that eating one common 'superfood' could cut Alzheimer's disease risk by almost 50%
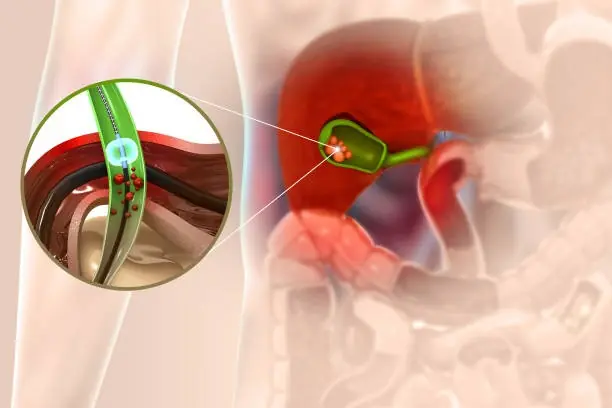
Side Effects and Dietary Recommendations Post Gallbladder Surgery

Signs You May Be Living With High-Functioning Anxiety

How to Know if You Have Fibromyalgia + 8 Natural Approaches to Relieve
Dark eye circles might be a subtle health warning

Could This 3D-Printed ‘Electronic Glove’ Keep Your Heart Beating Forever?

The Amount Of Time You Spend Peeing Could Be A Warning Sign For Bigger Health Issues

Scientists may have finally developed pill to cure deadly disease with 90% mortality rate
Man Shares His 'Proof' of Life After Death and the Seven 'Stages' of the Afterlife

Dental Expert Reveals the Top Two Brushing Mistakes That Lead to Yellow Teeth

They Hid This From Seniors: It Unclogs Arteries INSTANTLY!
This Secret Herb Can Heal 20 Diseases
Research shows that individuals who took psilocybin experienced significant enhancements in emotional empathy.

New Study Investigates Why Vaping Could Be More Dangerous Than Smoking

Disturbing X-ray Shows Creatures Breeding Inside Man's Body After Everyday Kitchen Mistake
Foods you should not eat every day because they can easily cause diabetes

New Study Reveals Hidden Dangers Lurking in Your Bottled Water
News Post

7 Warning Signs of Liver Damage You Shouldn’t Ignore
Chewing Gum Releases Microplastics Into Saliva – Even Natural Gums Are Not Safe, Study Finds
STUDY SHOWS SWITCHING TO PERSONAL CARE PRODUCTS WITHOUT CERTIAN PRESERVATIVES TURNS BREAST CANCER GENES OFF IN 28 DAYS
Study finds that eating one common 'superfood' could cut Alzheimer's disease risk by almost 50%

I Became a Burden to My Father after I Lost the Ability to Walk

I Was Stunned When the Teacher Said All the Kids Talked about How Amazing My Husband Was on Father's Day, I'm a Widow
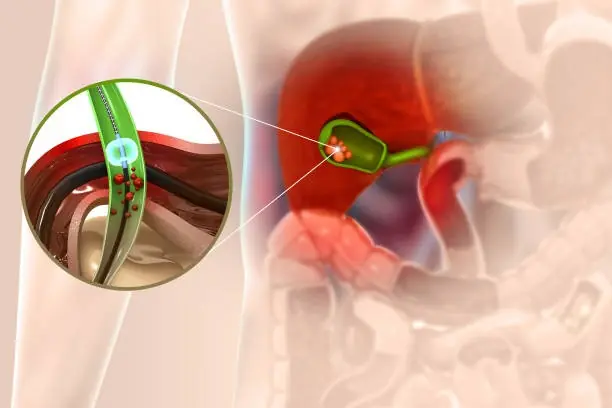
Side Effects and Dietary Recommendations Post Gallbladder Surgery
I Bought a Vintage Blazer at a Thrift Store for My Mom, But the Note Inside Revealed a Secret She Kept for 40 Years

Signs You May Be Living With High-Functioning Anxiety

How to Know if You Have Fibromyalgia + 8 Natural Approaches to Relieve
Dark eye circles might be a subtle health warning

Could This 3D-Printed ‘Electronic Glove’ Keep Your Heart Beating Forever?

My Neighbor Drove over My Lawn Every Day as a Shortcut to Her Yard

The Amount Of Time You Spend Peeing Could Be A Warning Sign For Bigger Health Issues

On the Day I Was Supposed to Marry the Love of My Life I Saw Her Leaving Town With My Father

Entitled Guest Demanded a Free Table at 'Her Friend’s' Restaurant — Too Bad I Was the Owner

Scientists may have finally developed pill to cure deadly disease with 90% mortality rate
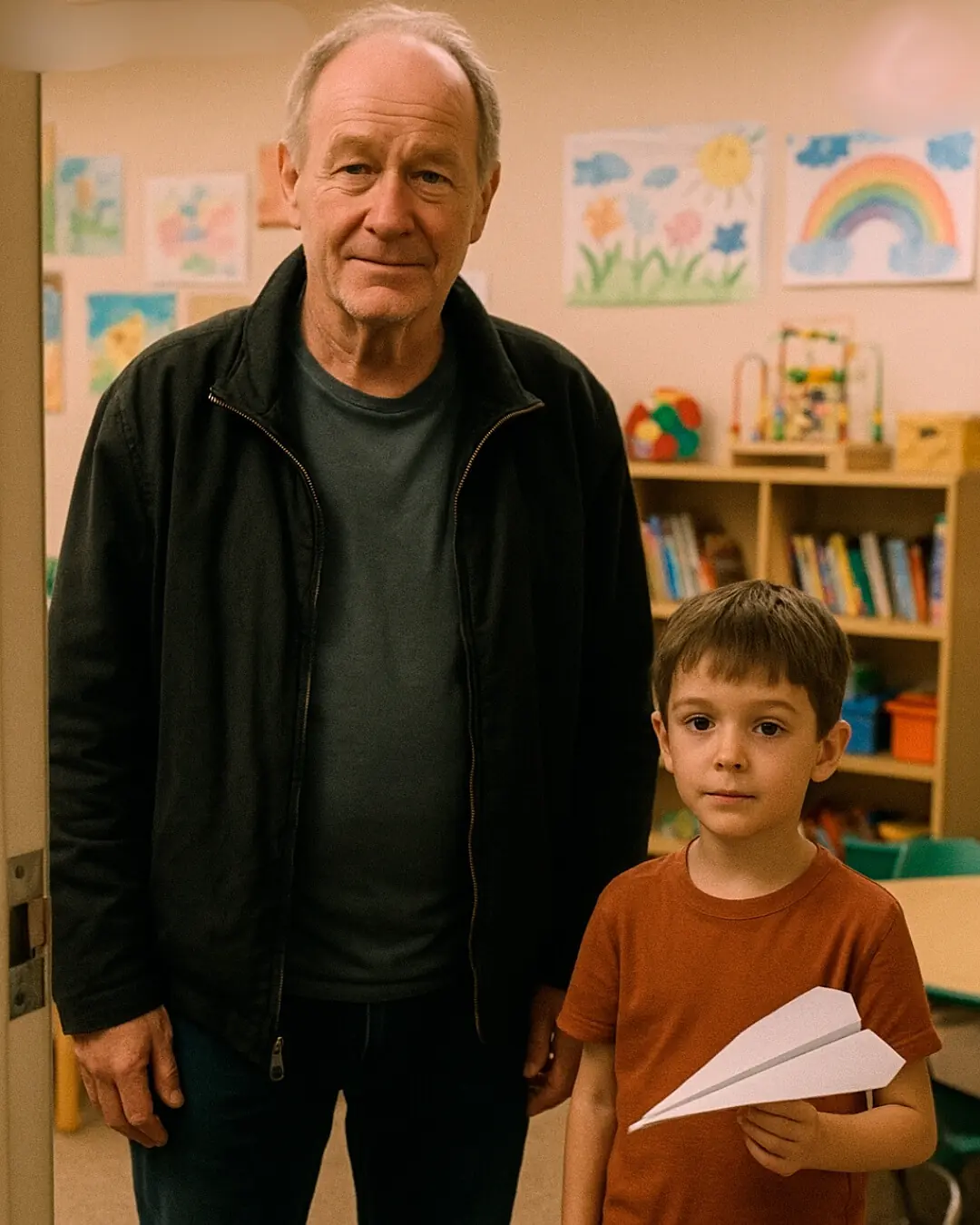
I Lost My Wife and Shut the World Out—Then an Orphaned Boy Opened My Heart Again

My Mom Avoided Me for Years—I Decided to Surprise Her Without Warning and Was Shocked by What She'd Been Hiding
