Scientists Have Discovered An Alarming Rise in Advanced Prostate Cancer in California

Rising Advanced Prostate Cancer Cases in California Spark Concern, UCSF Study Finds
A recent study conducted by researchers at the University of California, San Francisco (UCSF), has uncovered a troubling increase in advanced prostate cancer diagnoses across California over the past decade. Experts link this surge to changes in national screening guidelines, which have led to fewer men undergoing routine prostate cancer screenings. Although this trend has been observed across the U.S., the increase is significantly steeper in California, where the rate of advanced cases has surpassed the national average.
At the same time, after years of steady decline, prostate cancer death rates in most parts of the state have now plateaued, raising alarms among public health experts. These findings underscore the complex challenge healthcare providers face: finding the right balance between early detection and minimizing overtreatment—a dilemma that continues to influence prostate cancer screening policies and practices.
The study, published on January 27 in JAMA Network Open, emphasizes the critical need for more effective screening approaches. These methods must be capable of identifying dangerous, life-threatening cancers while avoiding the unnecessary diagnosis and treatment of slow-growing tumors that are unlikely to ever pose serious health risks.
A Growing Statewide Concern Across All Communities
“This overall rising trend is alarming and has occurred across all age groups, geographic regions, and racial and ethnic backgrounds in California,” said Dr. Erin L. Van Blarigan, ScD, an associate professor of Epidemiology, Biostatistics, and Urology at UCSF and the study’s lead author.
“Our data clearly show how urgent this issue is becoming,” she added. “The challenge for researchers and clinicians is identifying a screening strategy that catches aggressive cancers early without contributing to overdiagnosis and overtreatment. When men don’t get screened, the number diagnosed with late-stage prostate cancer—when treatments are much less effective—rises quickly.”
Navigating the Risks and Benefits of Prostate Cancer Screening
Prostate cancer remains the most commonly diagnosed cancer among men in the United States and is the second-leading cause of cancer-related death. However, not all prostate cancers behave the same way. While some are highly aggressive and fast-growing, many are indolent, meaning they grow slowly and may never cause symptoms or require treatment during a man’s lifetime.
The most frequently used screening method, the prostate-specific antigen (PSA) blood test, can help detect early signs of prostate cancer. However, PSA tests cannot reliably distinguish between aggressive and non-aggressive forms of the disease. As a result, some men may be diagnosed with low-risk cancers and undergo invasive treatments—such as surgery or radiation—that come with significant side effects, including urinary incontinence and erectile dysfunction.
On the flip side, avoiding screenings altogether carries its own risk. Some aggressive cancers may not be identified until they reach advanced stages, when treatment options are more limited and outcomes are significantly worse.
For many years, PSA screening was recommended as a routine procedure for most men. However, in 2012, the U.S. Preventive Services Task Force (USPSTF) advised against routine PSA screening for all men, aiming to reduce unnecessary treatments. This controversial decision prompted a nationwide drop in screening rates. In 2018, the USPSTF revised its stance, recommending that men aged 55 to 69 engage in shared decision-making with their doctors to weigh the potential benefits and risks of screening.
Despite this updated guidance, a large number of men—especially those in underserved communities or at higher risk—are not having these critical conversations with their healthcare providers, potentially missing opportunities for early detection and timely treatment.
California’s Prostate Cancer Trends: A Closer Look
The UCSF study analyzed data from nearly 388,000 men diagnosed with prostate cancer in California between 2004 and 2021. Of those, nearly 28,000 (7.2%) were diagnosed with advanced-stage disease, which has a five-year survival rate of just 37%.
Key insights from the study include:
-
Advanced prostate cancer rates in California remained stable or declined slightly until 2010. Starting in 2011, however, rates began to rise by 6.7% annually through 2021.
-
In contrast, the national average increased at a slower pace—by about 4.5% per year from 2011 to 2019.
-
The fastest regional growth in California was observed in the Central Coast, with a 9.1% annual increase, while the slowest was in the Southern San Joaquin Valley at 2.3%.
-
Prostate cancer death rates dropped by 2.6% per year between 2004 and 2012 but then leveled off in 7 out of 10 regions across the state.
-
The highest mortality rates were recorded in the Inland Empire, followed by San Diego-Imperial and the North Coast. The San Francisco Bay Area reported the lowest mortality rates.
These regional disparities point to differences in healthcare access, screening practices, environmental factors, and public awareness, all of which may influence prostate cancer outcomes.
The Importance of Continued Research and Adaptive Screening Policies
The findings highlight a pressing need for ongoing surveillance and research into how screening recommendations are impacting different communities. Experts stress that this data is essential for developing more personalized and effective strategies moving forward.
“It’s important to continue monitoring prostate cancer trends both in California and nationally,” said Dr. Scarlett L. Gomez, PhD, MPH, senior author of the study and a professor at UCSF’s Department of Epidemiology & Biostatistics. “Understanding how these shifts in policy affect various populations can guide future improvements in prevention, diagnosis, and treatment.”
Advancements in genetic testing, imaging technology, and biomarkers offer promising new tools for identifying high-risk individuals more precisely. These innovations may allow doctors to better determine who would benefit from screening and who might safely avoid it, helping to reduce unnecessary procedures and improve patient outcomes.
What This Means for Men’s Health Going Forward
This research adds to the growing body of evidence that prostate cancer screening needs to be more nuanced, targeted, and inclusive. It underscores the importance of ongoing education for both patients and healthcare providers.
Men, particularly those with a family history of prostate cancer or who belong to high-risk demographic groups, are encouraged to have open, informed conversations with their physicians about screening options. These discussions should take into account each individual’s risk factors, personal values, and preferences.
Ultimately, the goal is to ensure that life-threatening cases are caught early, while avoiding the harm of overtreatment for cancers that would not have progressed. As researchers continue to refine screening tools and guidelines, there is hope that men’s health outcomes will improve, and future trends will show a decline in advanced-stage diagnoses.
The study, titled “Trends in Prostate Cancer Incidence and Mortality Rates,” was published in JAMA Network Open and funded by the California Department of Public Health, the Centers for Disease Control and Prevention’s National Program of Cancer Registries, and the National Cancer Institute’s SEER Program.
News in the same category


This Is What Happens To Your Body When You Smoke Weed And Work Out

The Hidden Meaning Behind Wearing an Ankle Bracelet—Most People Have No Idea
How to Safely Remove Milia

Natural Methods to Destroy Bloating and Heartburn-Causing Bacteria in Your Gut
Doctor warns of the worrying symptoms that mean common disorder could actually be bowel cancer

15 Early Signs Your Body is Fighting Cancer
common morning habits that may increase your risk of stroke
New COVID Wave Surges — Health Officials Sound Alarm As Cases Double

How to Improve Your Vision Naturally with One Simple Ingredient: Saffron

How to STOP Cravings FAST Without Dieting! (The Natural Ozempic?)

Doctors make disturbing discovery in the brains of heavy alcohol drinkers that 'can cause long-term effects'

World-first sperm race is happening soon and the creators have revealed how it will work

Scientists Grow First Fully Formed Tooth In Lab — A Groundbreaking Breakthrough

New COVID Wave Surges — Health Officials Sound Alarm As Cases Double

10 Things That Men May Find Unattractive About Women Over 50
8 Signs You Might Be Affected by Lactose Intolerance
Understanding Diabetes: Types, Symptoms, Risks, and How to Manage It
Doctors Highlight A Rare Cancer Symptom That Can Appear On Your Toenails
News Post

Diet and Uric Acid: Foods to Avoid for Gout Prevention

This Is What Happens To Your Body When You Smoke Weed And Work Out

My Husband Took His Female Colleague to My Inherited Lake House for 'Business Trips' — But He Had No Idea I’d Already Installed Cameras
MIL Billed Me $3,360 for Babysitting Her Own Grandson — Here's How I Settled the Score
I Was Forced to Pay Rent to My Future MIL Just to Stay in Her House and Keep My Relationship Alive

Our Sassy Neighbor Threw a Party in Our Backyard, Demanding We Stay at Home, but We Had the Last Laugh

The Hidden Meaning Behind Wearing an Ankle Bracelet—Most People Have No Idea

My Husband Called Me Lazy for Wanting to Quit My Job While 7 Months Pregnant – So I Taught Him a Lesson He'll Never Forget

After Their Son's Death, This Elderly Couple Stopped Cooking & Spent 20 Years Sharing Meals with Neighbors — Until One Neighbor's Rejection Broke Their Hearts
Husband Gifted Me a Mop on Our 10th Anniversary as His Sister Laughed – Moments Later, Karma Restored My Faith in Goodness

AM I WRONG FOR BEING UPSET THAT MY 71-YEAR-OLD MOM, ELEANOR, SPENT HER MONEY ON TRAVELING INSTEAD OF HELPING ME, SOPHIA, WITH MY BILLS?

My Husband Bought First Class Tickets for Himself and His Mom Leaving Me and the Kids in Economy - My Lesson to Him Was Harsh

My MIL Thought I Was Not Beautiful Enough for Her Son, So I Entered a Beauty Contest to Win the Crown
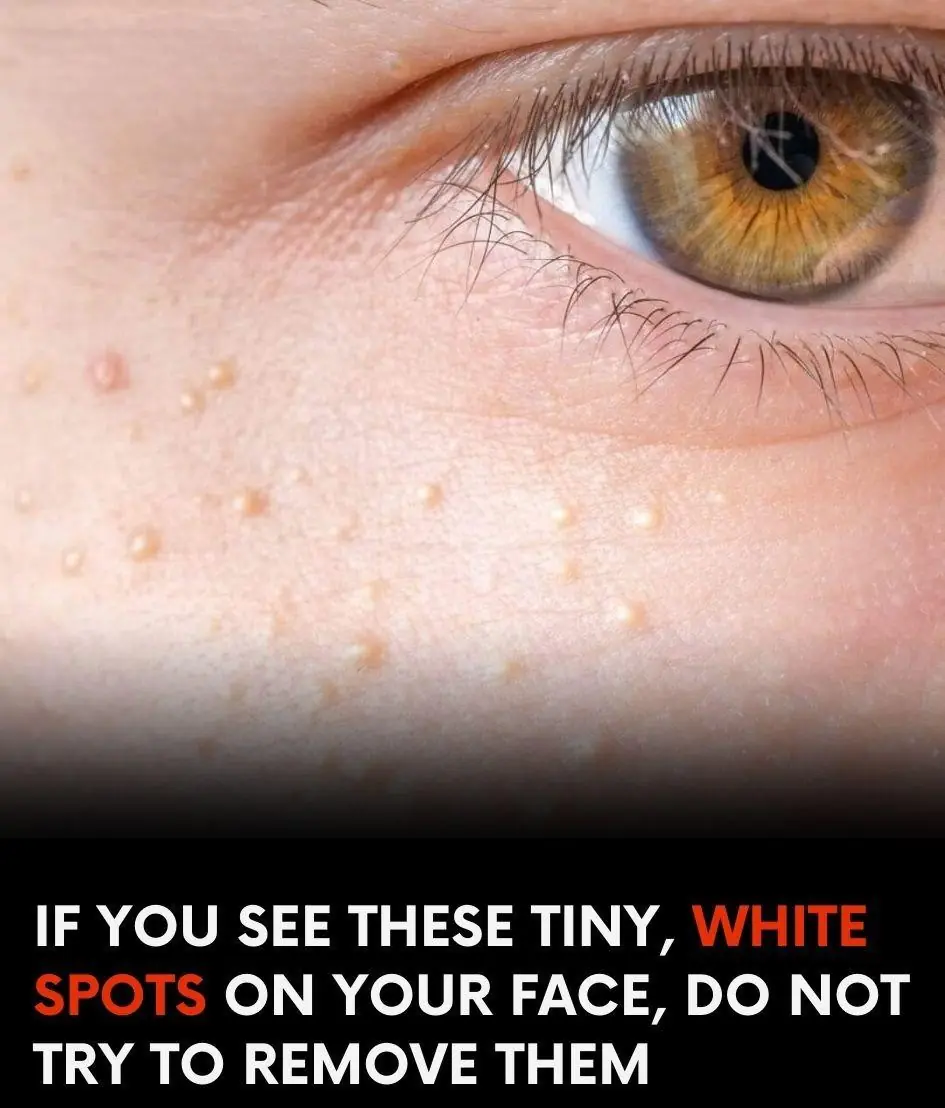
How to Safely Remove Milia

Natural Methods to Destroy Bloating and Heartburn-Causing Bacteria in Your Gut
Doctor warns of the worrying symptoms that mean common disorder could actually be bowel cancer

15 Early Signs Your Body is Fighting Cancer
common morning habits that may increase your risk of stroke