
🩺 Unusual Case of Sweet Syndrome Triggered by New Inhaler Therapy in Primary Care
A recent clinical case sheds light on a rare but clinically important adverse reaction that all primary care providers should be aware of: acute-onset Sweet syndrome following the use of a new inhaled therapy.
Inhalers are typically considered safe and well-tolerated for patients managing chronic obstructive pulmonary disease (COPD). However, this unusual case serves as a critical reminder that even routine medication adjustments can, on rare occasions, provoke unexpected immune-mediated responses — highlighting the need for continued vigilance in day-to-day prescribing.
Let’s delve into what happened, how the diagnosis was established, and why early recognition can make all the difference — empowering clinicians and patients alike to detect subtle but significant clinical signals.
Because real patient safety is about more than treating disease.
It’s about listening when the body speaks in surprising ways.
🔍 What Is Sweet Syndrome?
Sweet syndrome, or acute febrile neutrophilic dermatosis, is a rare inflammatory condition characterized by:
-
Sudden onset of painful, red to purple skin plaques or nodules
-
Typically associated with fever and elevated inflammatory markers
-
Histology shows a dense infiltration of neutrophils in the dermis — notably without vasculitis
This syndrome is classified as neutrophilic dermatosis, and while it is uncommon, its presentation can be dramatic and easily mistaken for infection, allergy, or even cellulitis.
🔍 Common Triggers Include:
-
✅ Infections
– Especially upper respiratory tract infections -
✅ Malignancies
– Often hematologic, such as acute myeloid leukemia (AML) -
✅ Autoimmune disorders
– Including lupus, inflammatory bowel disease (IBD) -
✅ Medications
– Such as G-CSF, certain antibiotics, and NSAIDs
📌 Notably, drug-induced Sweet syndrome is estimated to account for up to 12% of all cases — although most have been associated with systemic drugs, not inhaled therapies.
📋 Case Summary: A Surprising Reaction to an Inhaler Change
Patient Profile:
-
Age: 55-year-old female
-
Medical History: Hypertension, stable COPD
-
Baseline Therapy: Enalapril and formoterol (long-term use)
Clinical Context:
Due to worsening lung function, her pulmonologist opted to switch her from her long-standing formoterol inhaler to a dual bronchodilator: indacaterol/glycopyrronium, a combination of a long-acting beta-agonist (LABA) and a long-acting muscarinic antagonist (LAMA).
Presentation:
Within 48 hours of starting the new inhaler, she developed:
-
Rapid-onset, tender, and brightly erythematous plaques on the face and neck
-
Low-grade fever (37.9°C / 100.2°F)
-
No respiratory deterioration, joint pain, or mucosal lesions
-
Denied recent illness, new skincare products, or dietary changes
-
Reported recent sun exposure, but used SPF 50+ protection
She sought care in a primary care setting, concerned about a possible infection or allergic response.
🧪 Diagnostic Workup
-
Complete Blood Count (CBC): Normal WBC, mild neutrophilia
-
Inflammatory Markers: Elevated C-reactive protein (CRP) and ESR
-
Autoimmune Markers: ANA, ANCA, RF — all negative
-
Cultures: Throat swab and blood cultures — no infection found
-
Skin Biopsy: Dense neutrophilic infiltrate in the dermis without vasculitis
➤ Consistent with Sweet syndrome
✅ Final Diagnosis: Drug-induced Sweet syndrome, most likely triggered by the newly initiated inhaler (indacaterol/glycopyrronium).
💊 Why This Case Is Clinically Significant
While Sweet syndrome linked to systemic medications is well documented, this case may represent one of the first reported instances associated with an inhaled dual bronchodilator.
Neither indacaterol nor glycopyrronium has been previously linked to Sweet syndrome, but both have systemic absorption, even when administered via inhalation.
🔬 Hypothesized Mechanism:
-
Likely an immune-mediated hypersensitivity reaction
-
Possibly triggered via cytokine release or neutrophil activation
-
The rapid onset suggests immune priming rather than a delayed-type allergy
✅ Management & Outcome
Interventions:
-
Immediate discontinuation of the new inhaler
-
Reinitiation of previous formoterol inhaler
-
Oral prednisone: 40 mg/day for 5 days, followed by a taper
Result:
-
Skin lesions resolved within 72 hours
-
Fever subsided rapidly
-
No recurrence at 3-month follow-up
-
COPD stabilized on the previous inhaler with good control
The patient was advised to avoid re-exposure, and alternative therapies were considered for future adjustments, with plans for close monitoring.
🚨 Key Clinical Takeaways
-
✅ Monitor closely after any medication switch — even with inhaled therapies
-
✅ Consider Sweet syndrome in cases of sudden skin lesions + fever, even without systemic drug exposure
-
✅ Skin biopsy is crucial to distinguish from cellulitis, vasculitis, or other dermatoses
-
✅ Prompt discontinuation of the triggering agent leads to rapid resolution
-
✅ Thorough documentation helps prevent future re-exposure and supports post-marketing surveillance
❌ Debunking Common Misconceptions
-
❌ “Only systemic drugs can cause Sweet syndrome”
➤ False — inhaled medications can be systemically absorbed and trigger immune responses -
❌ “It’s just a rash — treat with antibiotics”
➤ Incorrect — misdiagnosis can lead to unnecessary treatment and delay resolution -
❌ “Sweet syndrome is contagious”
➤ Not true — it’s an inflammatory, non-infectious condition -
❌ “All rashes after inhaler use are allergies”
➤ Misleading — could be irritation, infection, or an immune-mediated reaction like this one
🩺 Final Thoughts
This case is a compelling reminder that even familiar, widely used treatments can carry unfamiliar risks. As we aim to optimize therapy for chronic conditions like COPD, it’s essential not only to follow guidelines — but to remain curious, observant, and responsive to patient-reported symptoms, however subtle they may seem.
While indacaterol/glycopyrronium remains a safe and effective therapy for the vast majority of COPD patients, clinicians should be aware of the potential — however rare — for adverse cutaneous immune reactions.
Because medicine isn’t just about protocols.
It’s about patterns. Listening. And acting early.
And sometimes, the most powerful tool in medicine?
Clinical curiosity — guided by compassion.
News in the same category


The #1 Drink to Prevent Foamy Urine — Plus 7 More Your Kidneys Will Thank You For

The #1 Most Effective Remedy for Dental Plaque (And How to Beat Tartar at Home)

JUST 1 CUP FLUSHES POUNDS OF TOXIC WASTE

Just 2 Nuts a Day Can Support Your Thyroid, Help With Weight Loss, and Balance Blood Sugar

Zinc Deficiency Triggers Inflammation in Your Body — Here’s What to Eat to Fix It
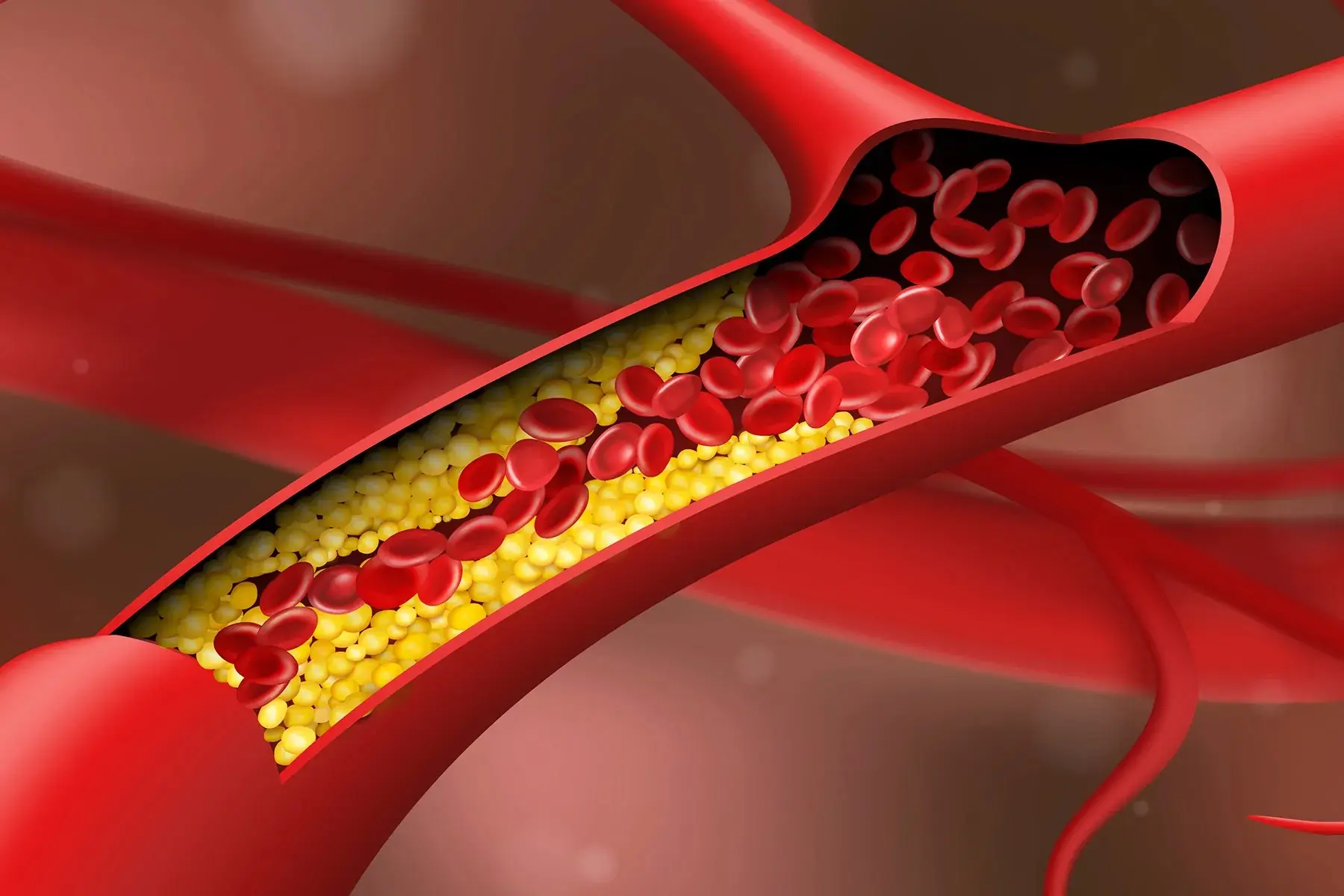
CLEANSE CLOGGED ARTERIES WITHOUT MEDICATION
The #1 Way To Stop Bloating Fast

6 warning signs of a clogged artery most people ignore (cardiologist alert)
Foot Symptoms That Could Signal Kidney Problems
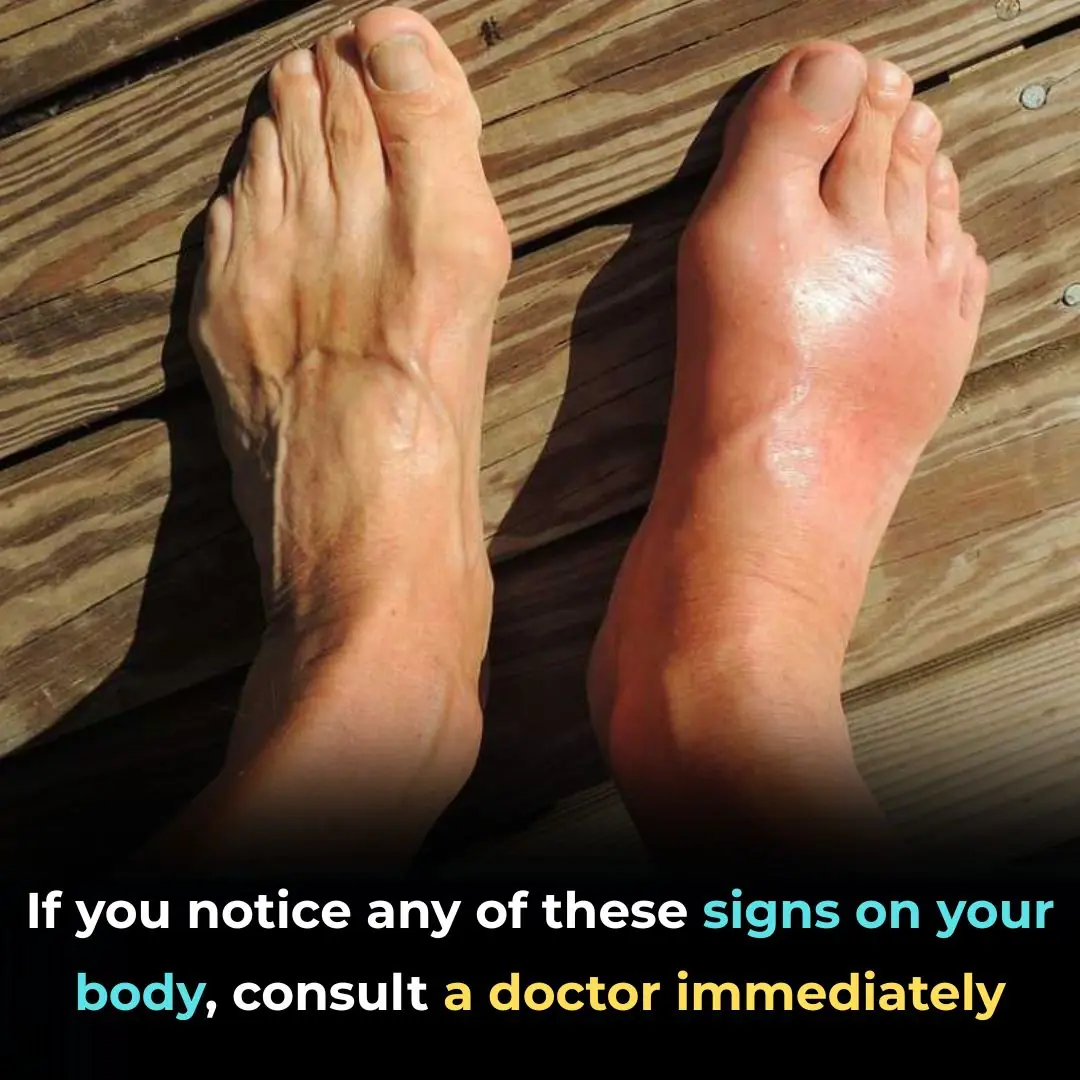
Redness Swelling and Warmth in One Leg

These are the signs that he is...read more

12 weird signs your body isn’t making enough bile—don’t ignore these!

12 Fish Species You Need to Know to Avoid

🦴 The Vitamin & Mineral Deficiencies That May Be Behind Leg and Bone Pain

Tomato Benefits for Skin – Rub Tomato Slice on Face

Hidden Dangers on Your Plate: 4 “Clean” Foods That Can Secretly Harm Your Health
4 Unusual Signs in Your Neck That Could Be Symptoms of Cancer — Don’t Ignore Them

6 Warning Signs in Your Legs That Could Indicate a Serious Disease — Don’t Ignore Them
News Post
Growing Concern Over Visceral Fat — Doctors Recommend 9 Foods to Help Burn It Naturally

7 Amazing Health Benefits of Banana Blossoms

Bryophyllum Calycinum (Kalanchoe Pinnata): Benefits and Uses

Purslane: The Superfood That Tastes Better Than Meat – 7 Reasons to Grow It in Your Garden
7 Benefits of Chewing Raw Garlic on an Empty Stomach

Chayote Remedy: Natural Cure for Pain, Swelling, Blood Pressure & Cholesterol
Alkaline Water – Recipe and Health Benefits for Skin & Hair

Garlic, Honey, and Cloves – a powerful natural remedy packed with health benefits

A Natural Blend of Rosemary, Cloves, and Bay Leaves

Ginger and Orange Detox Drink – Cleanse Kidneys, Liver, and Lungs Naturally

The Purple Maguey Plant — Benefits and Traditional Uses

Bananas, Garlic, and Dates: The Powerful Health Combo
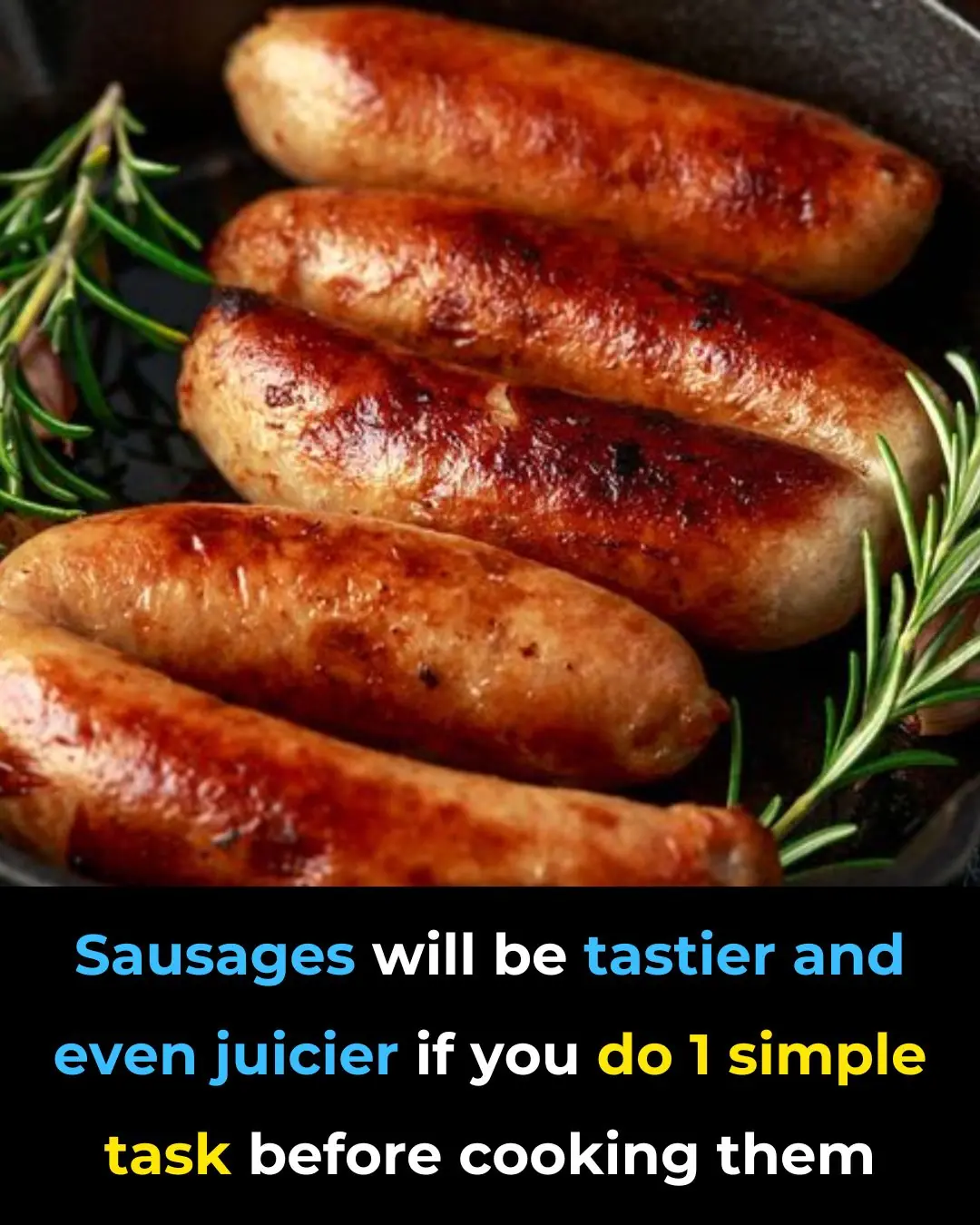
Make Your Sausages Juicier and More Flavorful With This One Simple Step Before Cooking
Don’t Leave Your Phone Charger Plugged In

“A Gift of Belief: How One Simple Act of Kindness Changed a Little Boy’s World”

Keep your bathroom clean and fresh all year round by applying these 7 small habits.
‘This Is An Opportunity For You To Get Some Portal Film’ | Deion Sanders’ Ruthless Scrimmage Urging Bench Players To Transfer Angers Fans
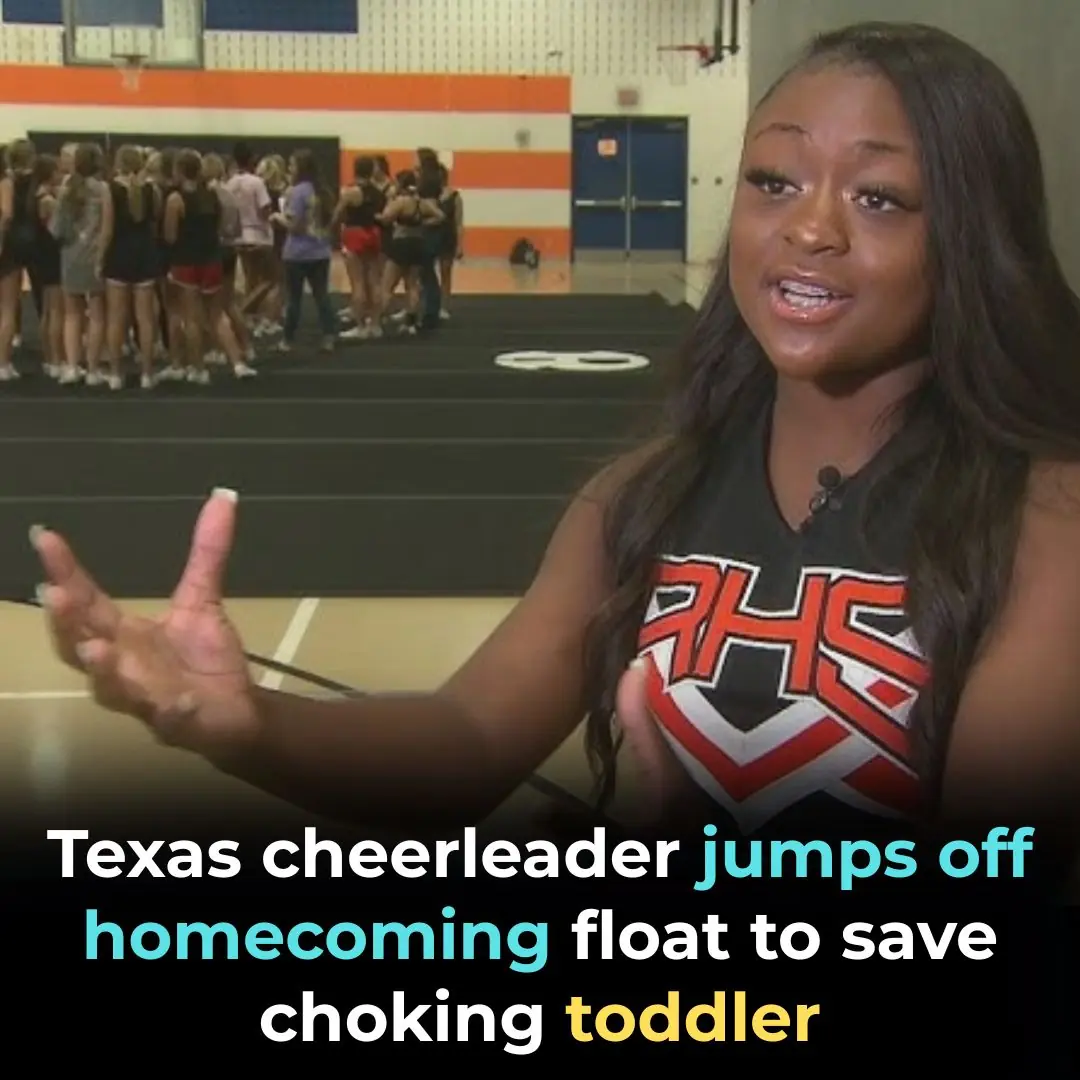
Texas Cheerleader Jumps Off Homecoming Float To Save Choking Toddler
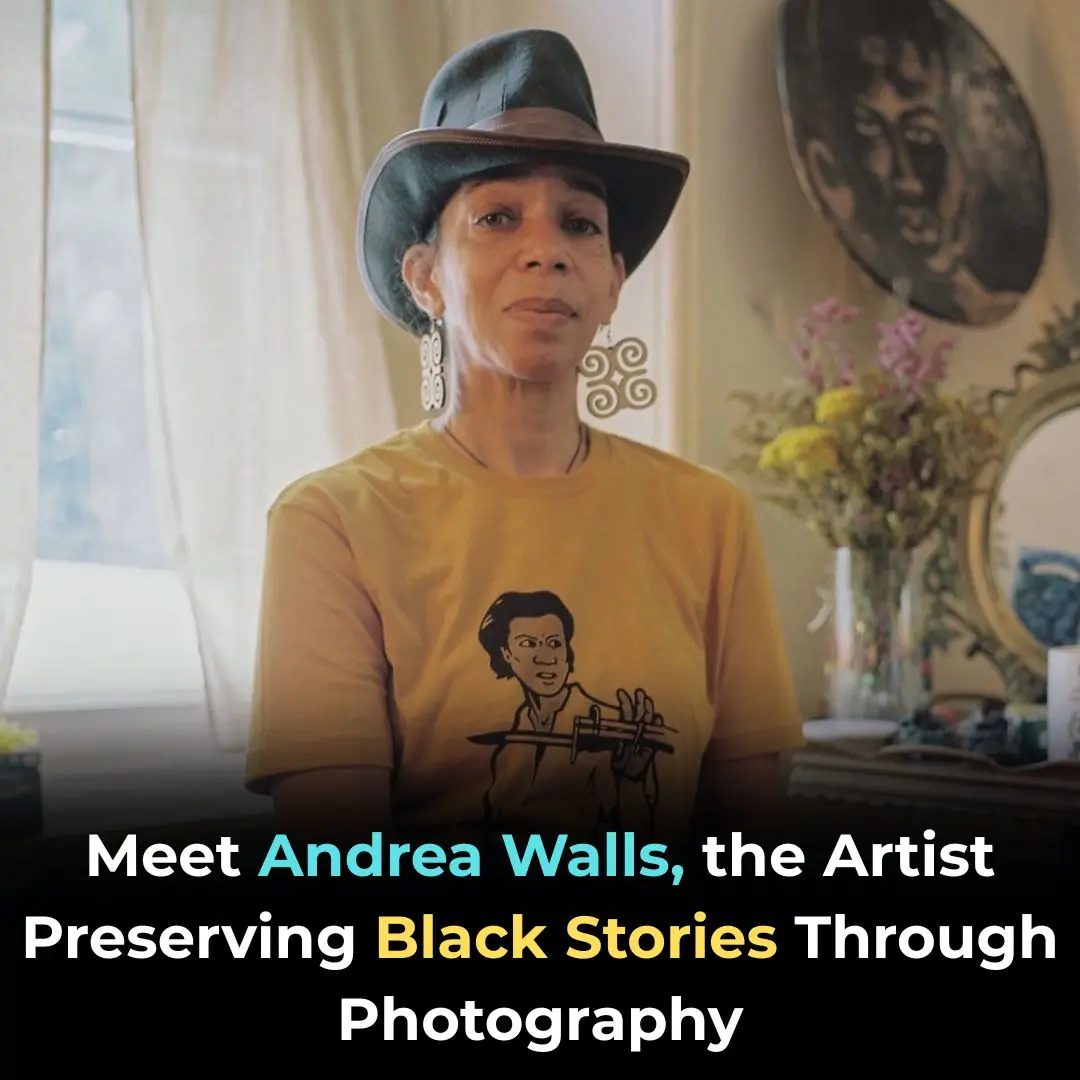
Meet Andrea Walls, the Artist Preserving Black Stories Through Photography
