This New ‘universal cancer vaccine’ trains the immune system to kill any tumor
A Universal mRNA Cancer Vaccine: A Potential Breakthrough in Oncology
A research team at the University of Florida has developed an experimental mRNA-based vaccine that could transform the way cancer is treated. Unlike current cancer vaccines, which typically target a single tumor type or require costly, patient-specific customization, this innovative “universal” vaccine is designed to activate the immune system against any form of cancer.
In early preclinical studies, the vaccine not only enhanced the effectiveness of standard immunotherapy drugs but, in some cases, eliminated tumors entirely without additional treatments. This groundbreaking approach builds upon the same principles behind COVID-19 mRNA vaccines but repurposes them with a different mission: to make cancer cells more visible to the immune system and easier to destroy.
Early results in animal models are highly promising, hinting at a future where this vaccine could become a widely available alternative—or powerful complement—to traditional treatments such as surgery, chemotherapy, and radiation. While human trials are still ahead, this research signals a future where fighting cancer could become faster, less invasive, and more effective across diverse patient populations.
How the “Universal Cancer Vaccine” Works
Researchers at the University of Florida designed this mRNA-based vaccine to help the immune system detect, target, and eliminate cancer cells—regardless of the tumor type. Unlike traditional cancer vaccines that focus on a specific protein unique to one cancer, this universal strategy trains immune cells to mount a broad, virus-like response against tumors in general.
The vaccine uses lipid nanoparticles, a technology similar to that used in COVID-19 vaccines, to deliver strands of messenger RNA (mRNA) into the body. Instead of instructing cells to produce a viral protein, the mRNA directs cells to generate proteins such as PD-L1, which are associated with cancer cells but often hidden from immune surveillance. By artificially increasing PD-L1 expression within tumors, the vaccine essentially tags the cancer, signaling T cells to attack and destroy these cells more efficiently.
In mouse models, this approach has already yielded striking results. The vaccine not only worked in tandem with existing checkpoint inhibitor therapies, like PD-1 inhibitors used for drug-resistant melanoma, but in some instances, it eradicated tumors without any additional intervention. By focusing on immune readiness rather than individual tumor markers, this strategy could dramatically simplify and scale cancer vaccine technology.
According to Dr. Duane Mitchell, a co-author of the study, this method could pave the way for an “off-the-shelf” cancer vaccine—one that does not need to be custom-built for each patient but still delivers a potent and targeted immune response.

A New Era in Cancer Treatment
For decades, cancer treatment has largely relied on surgery, chemotherapy, and radiation therapy. While these approaches have saved millions of lives, they are often invasive, taxing, and come with significant side effects. Worse, many cancers eventually recur.
Over the last two decades, immunotherapy has emerged as a fourth pillar of cancer treatment. By harnessing the body’s own immune system, therapies like checkpoint inhibitors and CAR-T cell therapy have significantly improved outcomes for certain cancers, including melanoma and specific types of blood cancer. However, these treatments are far from universal. Many patients do not respond, and tumors often evolve mechanisms to evade immune detection.
Personalized cancer vaccines have been one proposed solution, using the genetic profile of a patient’s tumor to create a tailored vaccine. Although promising, this method is time-consuming, expensive, and not widely accessible. The University of Florida’s universal vaccine offers a fundamentally different approach: instead of tailoring treatment for each individual, it stimulates a generalized yet potent immune response, making it possible to treat a wide spectrum of cancers more efficiently.
Early laboratory evidence suggests this universal vaccine could serve as both a stand-alone therapy and a powerful complement to existing treatments. For example, in melanoma models resistant to PD-1 inhibitors, the vaccine re-sensitized tumors, enabling the drugs to work again. Similar effects were observed in mouse models of brain, skin, and bone cancers, where the vaccine sometimes eliminated tumors without any additional intervention.
Why PD-L1 Targeting Is a Game Changer
One of the most powerful defense mechanisms tumors use to avoid detection is the PD-1/PD-L1 pathway. PD-L1 proteins on tumor cells bind to PD-1 receptors on T cells, sending a “stand down” signal that effectively tells the immune system to ignore the cancer.
Checkpoint inhibitor drugs disrupt this signal by blocking PD-1 or PD-L1, but their success depends on whether the tumor is already expressing PD-L1. Tumors without PD-L1 expression often remain invisible, rendering these drugs ineffective.
The universal mRNA vaccine addresses this challenge by inducing PD-L1 expression directly within tumors, even those that were previously “invisible.” This shift enables a stronger, more coordinated immune response and enhances the effectiveness of checkpoint inhibitors. Because many cancers share these immune-evasion tactics, the vaccine’s broad approach could theoretically apply to multiple cancer types, making it a true universal platform.

Remaining Challenges and Next Steps
Despite these encouraging results, this vaccine remains in the preclinical phase. Human biology is significantly more complex than animal models, and many promising therapies have failed during clinical trials. The next steps include rigorous phase I human trials to evaluate safety, identify optimal dosing, and monitor real-world effectiveness.
Researchers will also need to determine the duration of immune activation provided by the vaccine and whether periodic boosters will be necessary. Safety is another key concern: because this vaccine broadly stimulates immune activity, there’s a potential risk of autoimmune reactions or unintended inflammation in healthy tissues. Fortunately, mRNA technology allows for relatively rapid adjustments to the formulation, a flexibility demonstrated during the rapid updates of COVID-19 vaccines.
The University of Florida team is now refining its formulations, testing alternative delivery mechanisms, and expanding research into cancers that are notoriously resistant to immune-based treatments, such as pancreatic and ovarian cancers. If early human trials show safety and efficacy, the vaccine could potentially move through regulatory channels more quickly, leveraging the manufacturing and distribution frameworks established during the pandemic.
Experts caution, however, that even under accelerated timelines, it will likely take several years before this vaccine could become widely available.
Supporting Your Immune System While Waiting
While a universal cancer vaccine could reshape the oncology landscape, it is still years away from clinical use. In the meantime, individuals can take evidence-based steps to strengthen their immune system and support overall health.
-
Stay current with screenings: Regular tests like mammograms, colonoscopies, Pap smears, and low-dose CT scans for high-risk smokers can detect cancers early, when they are most treatable.
-
Maintain a nutrient-rich diet: Fruits, vegetables, whole grains, legumes, and lean proteins help supply antioxidants, vitamins, and minerals essential for immune function.
-
Stay active: Moderate physical activity, such as 30 minutes of brisk walking most days, helps regulate immune responses and reduces systemic inflammation.
-
Avoid tobacco and limit alcohol: Both habits are linked to increased cancer risk and reduced immune efficiency.
-
Manage chronic conditions: Keeping conditions like diabetes, hypertension, and obesity under control reduces cancer risk and supports better treatment outcomes if cancer develops.
-
Prioritize sleep and stress management: Adequate rest and techniques such as meditation or yoga can help balance immune activity and support long-term health.
The Takeaway
The development of a universal mRNA-based cancer vaccine marks a significant leap forward in the fight against cancer. By exposing tumors through induced PD-L1 expression, this technology not only enhances the effectiveness of existing therapies but also shows potential as a stand-alone treatment.
If human trials validate its safety and efficacy, this innovation could usher in a future where cancer treatment is faster, less invasive, and more widely accessible—potentially reducing the need for chemotherapy, radiation, and even some surgeries.
Until then, the best course of action is to stay informed through reliable sources, adhere to evidence-based cancer prevention guidelines, and consider participating in clinical trials when eligible. Public awareness and engagement are key to turning groundbreaking research like this from a laboratory concept into a lifesaving reality.
News in the same category


David Quammen, the COVID Predictor Warns of New Pandemic Threats

YouTuber shows crazy impact running 5k every day as a total beginner has on your body
Chilling moment Google's Gemini broke father out of delusion that he was 'changing reality' from his phone
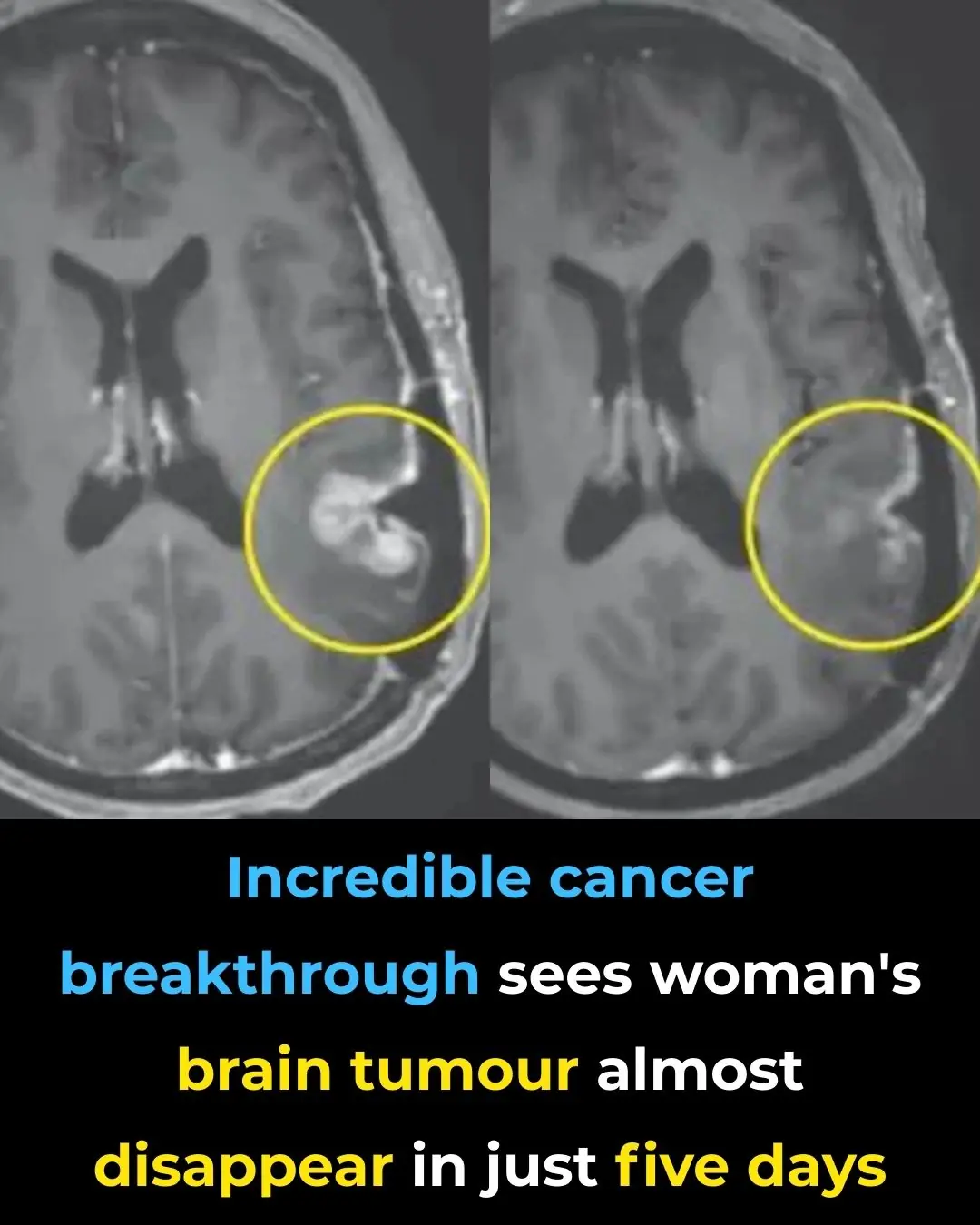
Incredible cancer breakthrough sees woman's brain tumor almost disappear in just five days

NASA astronaut's heartbreaking statement from ISS moments before finally returning to Earth

Beware of the Plastic Bottle Scam: A New Car Theft Tactic
Former PlayStation CEO reveals key way consoles could be cheaper in the future

Swarm of angry jellyfish force nuclear power plant to immediately shut down

The TwoDaLoo Double-Sided Toilet (A Couples Toilet That’s Not For Me… Us)

Jeff Bezos reportedly 'obsessed' with making wife Lauren Sanchez the next Bond girl

Final straw that led to billionaire CEO's desperate escape from Japan inside 3ft box
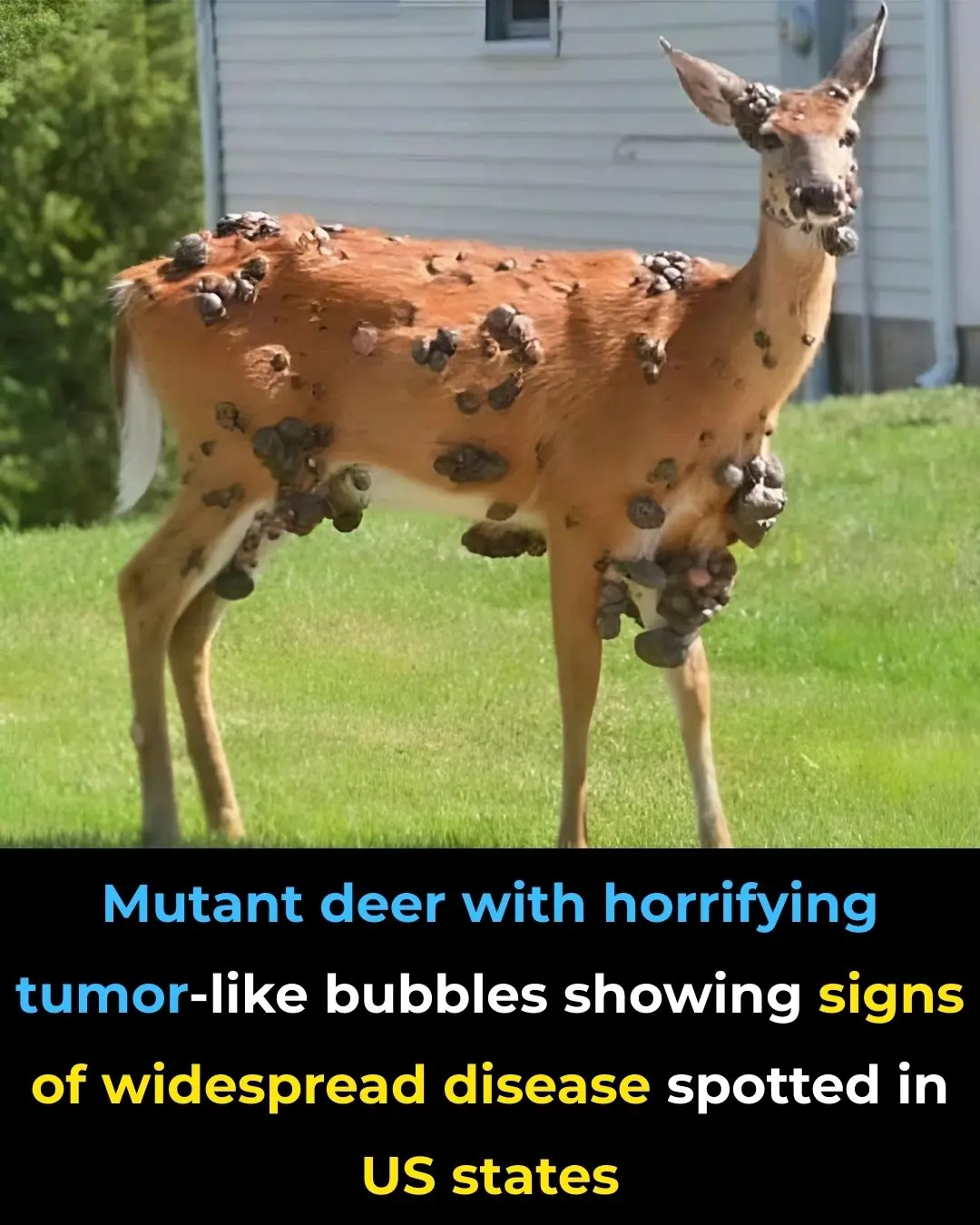
Mutant deer with horrifying tumor-like bubbles showing signs of widespread disease spotted in US states

'Frankenstein' creature that hasn't had s3x in 80,000,000 years in almost completely indestructible

Angelina Jolie’s ‘Zombie Lookalike’ Revealed As She Leaves Jail After Fooling Everyone

Japanese “Baba Vanga” Meme Resurfaces After July 2025 Tsunami Triggers Alerts

Cancer patients in England to be first in Europe to be offered immunotherapy jab

US assassin caught on CCTV faces lengthy prison sentence over failed murder plot
News Post
Sip these 5 powerful drinks for stronger kidneys
1 cup to destroy inflammation, clear mucus & unclog sinus, chest, and lungs!

Red Spots on Skin: Causes, Treatments, and More (Extensive Guide)

Why a Cat Rubs Against You

True Meaning When Black Butterflies Visit You

7 Warning Signs You May Have Uterine Fibroids

Parasite Cleanses: Do They Really Improve Your Gut Health — and Are They Safe?

8 Teas to Drink for a Healthier Body and Mind

The Hidden Truth About Tinnitus: Why That Ringing in Your Ears Shouldn’t Be Ignored
Over time, repeated noise trauma damages tiny hair cells inside the cochlea, which cannot regenerate, resulting in permanent hearing changes and tinnitus.

DIY Turmeric & Ginger Shots to Fight Inflammation, Boost Immunity & Soothe Your Gut

Coconut water: Is It Good for You, Nutrition, Benefits, Side Effects (Science Based)

Clean Arteries: 10 Foods to Eat Daily

10 Warning Signs of Parasites in Your Body
Diet and Uric Acid: Foods to Avoid for Gout Prevention

Hiker Encounters Massive Snake Camouflaged Along South Carolina Creek

8 Foods That Help Eliminate Cancer Cells

David Quammen, the COVID Predictor Warns of New Pandemic Threats
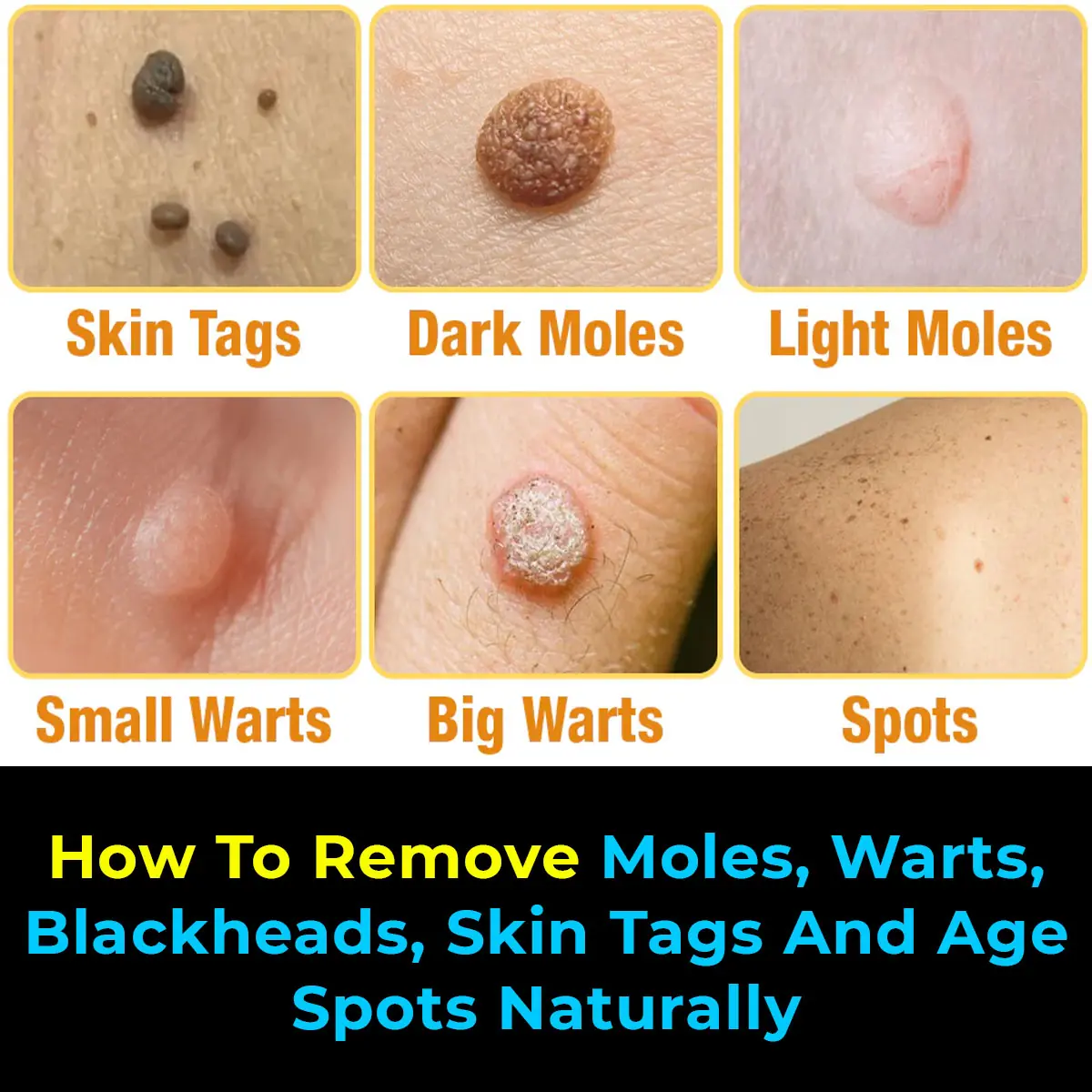
Natural Remedies to Address Skin Tags, Warts, and Blackheads
Tips for Selecting Fresh Pork at the Market