A French-made artificial heart brings new life to patients once dependent on donor transplants.
In a development that could reshape modern cardiology, researchers in France have advanced an artificial heart designed for continuous, long-term function—potentially reducing dependence on scarce human donors and redefining treatment options for severe heart disease.
The device was developed by the French company Carmat and is engineered to closely mimic the behavior of a natural human heart, both mechanically and physiologically. It uses a sophisticated network of internal sensors and biocompatible materials to regulate blood flow dynamically, automatically adjusting output as a patient rests, experiences stress, or becomes physically active. This adaptive response allows the artificial heart to function in a way that closely mirrors normal human physiology, rather than delivering a fixed mechanical rhythm.
Unlike traditional heart transplants, the artificial heart does not rely on donor availability and significantly lowers the risk of immune rejection. Its design incorporates advanced materials intended to be compatible with human blood and tissue, reducing complications such as clot formation, bleeding, and inflammatory responses—problems that have historically limited the success of earlier artificial-heart technologies and ventricular assist devices.
The potential impact is substantial. Tens of thousands of patients worldwide suffer from end-stage heart failure but never receive a transplant due to donor shortages, age restrictions, or medical incompatibilities. Early recipients of the Carmat heart have reported improved cardiovascular stability and the ability to return to everyday activities, regaining a level of independence that was previously impossible with conventional mechanical support alone.
Beyond individual patient outcomes, the technology also raises important implications for healthcare systems. A reliable long-term artificial heart could reduce transplant waiting lists, ease pressure on donor networks, and standardize treatment for advanced heart failure across regions with limited access to organ donation programs.
While broader clinical trials and long-term survival data are still needed, the progress suggests a future in which permanent artificial hearts could become a viable and widely adopted alternative to transplantation. If validated at scale, this technology could fundamentally change how heart failure is treated—shifting care from donor-dependent solutions to engineered, life-sustaining replacements that offer patients a renewed chance at long-term survival and improved quality of life.
News in the same category
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes

Surprising Health Benefits of Purslane (Portulaca oleracea)

Rising Deaths From Stomach Cancer: Doctors Warn — See These 4 Abdominal Signs and Seek Medical Care Immediately

Australia is replacing animal testing with smarter, humane science
Cracked Egg in Your Carton? Here’s When It's Safe to Eat—And When to Toss

Scientists Restore Natural Hearing Using Stem Cells in a Historic Medical Breakthrough
Morning Swelling in Kidney Disease: What Your Body Is Trying to Tell You

Cancer May Show These 2 Warning Signs at Night — Everyone Should Be Aware
Coffee Consumption May Slow Biological Aging in Severe Mental Illness
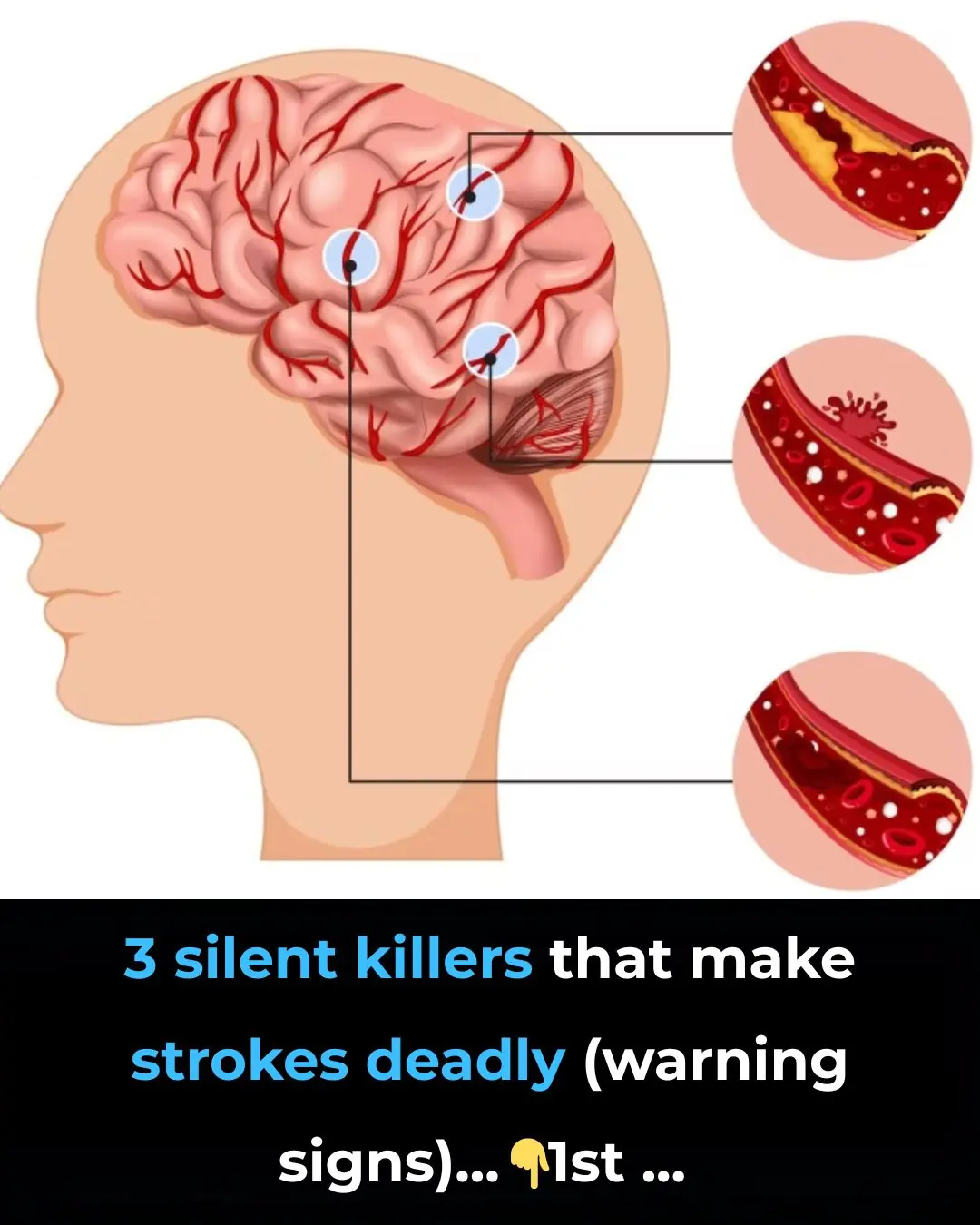
3 silent killers that make strokes deadly (warning signs)

You’d Be Surprised How Your Sleeping Environment Impacts Your Body and Mind

What To Know and Do About Pain Under Your Left Rib Cage
What Causes a Toenail To Turn Black?

Why So Many Women Wake Up With Bruises They Don’t Remember Getting
News Post
Advancing Clinical Excellence in IgA Nephropathy

3 types of fruits that are cheap in Vietnamese markets but are considered "pure gold" to protect health

Found this weird skin on my son's ear this morning. Doc appt is a week away. What can I do?

My nana taught me this hack to get rid of dark circles in 5 mins with 0 work. Here’s how it works
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes
Garlic with Olive Oil Over 50: The Irreversible Body Reaction Everyone’s Talking About

Discover How Baking Soda Could Transform Your Skin’s Appearance in Minutes – Even After 70!

What Happens When You Add Just 2 Garlic Cloves a Day to Your Routine – Even After 50!

13 Subtle Signs Your Kidneys May Need Attention

Stop Shaving? Exploring Popular Home Remedies for Hair Removal

Discover the Hidden Power of Ginger Oil: Why Women Over 65 Are Seeing Thicker, Darker Hair Naturally

Top 10 Foods That May Help Reduce Frequent Nighttime Urination (Nocturia)

Why Toothpaste and Baking Soda Aren’t the Answer for Wrinkles and Dark Spots – And What Might Help Instead
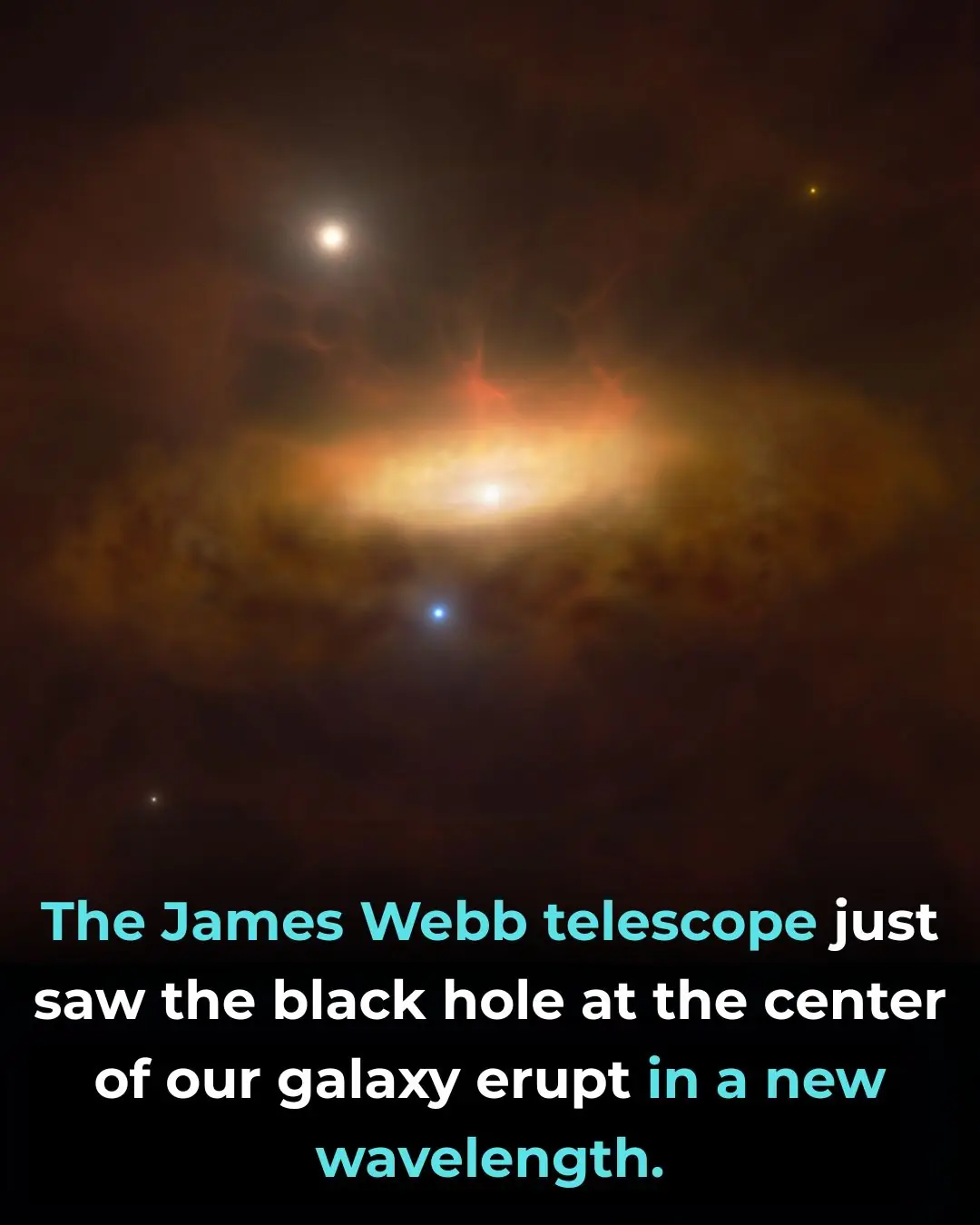
James Webb Space Telescope Reveals Hidden Mid-Infrared Flares from the Milky Way’s Central Black Hole
New Vision Correction Technique Reshapes the Cornea Without Surgery
Feeling Relieved Without Your Partner? A Psychologist Says It’s a Warning Sign
