Are Biologic Therapies Safe in Patients With Psoriasis and Cancer?
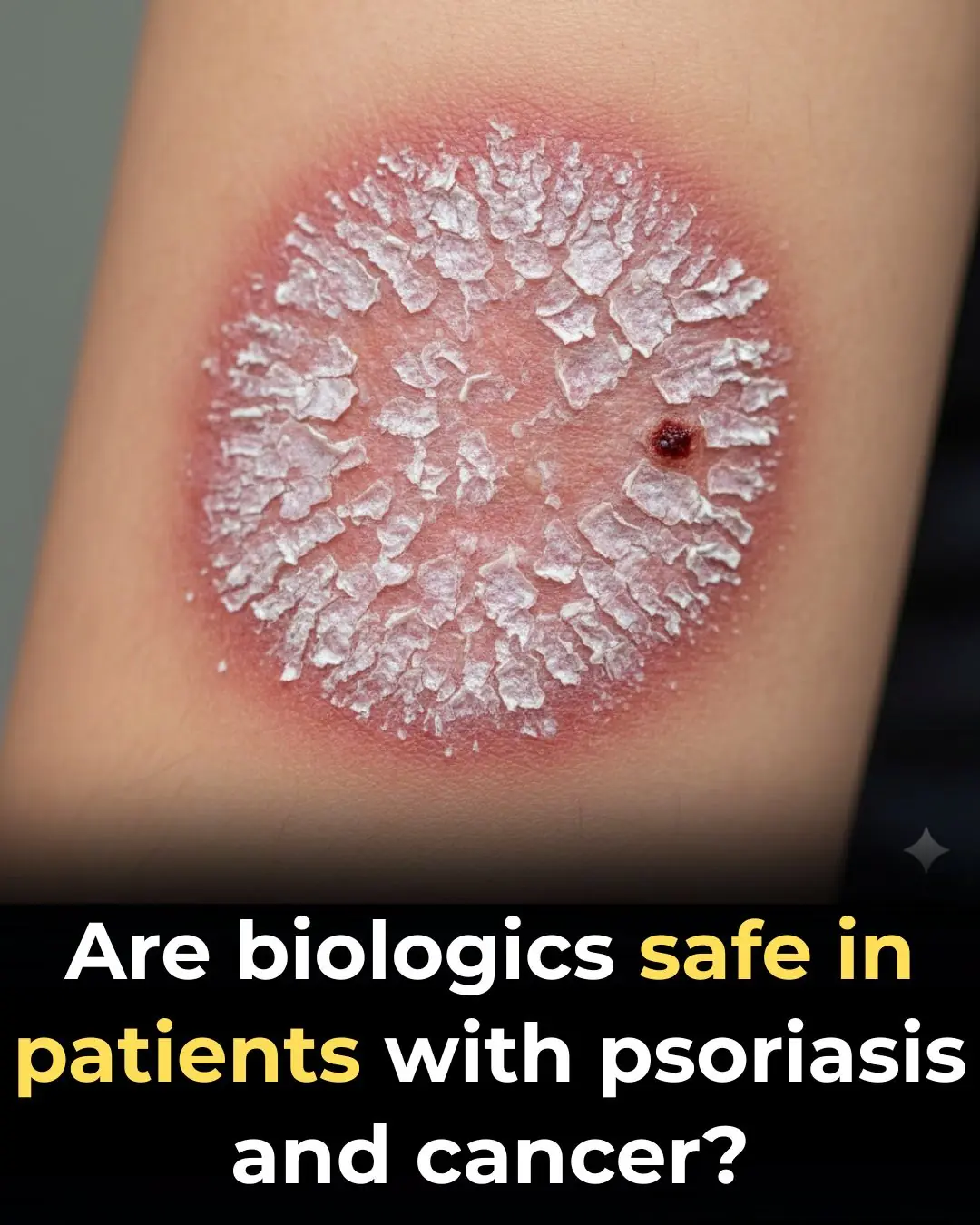
The management of moderate to severe psoriasis has been transformed over the past two decades by the advent of biologic therapies. These targeted agents have delivered unprecedented efficacy and improved quality of life for millions of patients. However, their use in individuals with active cancer or a recent history of malignancy has long remained a source of clinical uncertainty.
Concerns about immune modulation, tumor surveillance, and cancer recurrence have traditionally led clinicians to favor conventional systemic agents—or to delay treatment altogether—in this vulnerable population. New evidence now suggests that these fears may be overstated. Recent data indicate that biologic therapies demonstrate safety comparable to conventional systemic treatments in patients with psoriasis who have active cancer or a recent cancer history.
A Longstanding Clinical Dilemma
Psoriasis is a chronic, immune-mediated inflammatory disease that often requires systemic therapy for adequate control. At the same time, psoriasis patients may have an elevated baseline risk of certain malignancies due to chronic inflammation, shared risk factors, or prior exposure to immunosuppressive therapies.
Historically, biologics—particularly tumor necrosis factor (TNF) inhibitors—were approached with caution in patients with cancer because of their effects on immune pathways involved in tumor surveillance. As a result, many clinicians have relied on older systemic agents such as methotrexate, cyclosporine, or acitretin, despite their own well-documented toxicities.
New Evidence on Safety Outcomes
Recent observational studies and registry-based analyses provide reassuring data. In patients with psoriasis who had active malignancy or a recent cancer history, biologic therapies were associated with:
-
Comparable cancer progression rates
-
Similar cancer recurrence rates
-
No significant increase in overall malignancy-related adverse outcomes
Importantly, these outcomes were similar to those observed in patients treated with conventional systemic agents, suggesting that biologics do not confer additional oncologic risk in this context.
Understanding the Mechanisms
Modern biologic therapies target specific immune pathways—such as TNF-α, interleukin (IL)-17, IL-23, and IL-12/23—rather than broadly suppressing immune function. This targeted approach may explain why biologics do not appear to significantly impair anti-tumor immune surveillance compared with traditional immunosuppressants.
Additionally, newer biologics, particularly IL-17 and IL-23 inhibitors, may have a more favorable safety profile than earlier agents, further supporting their use in carefully selected patients with cancer histories.
Comparison With Conventional Systemic Therapies
Conventional systemic agents have long been considered the “safer” option in patients with cancer, yet they are not without risks:
-
Methotrexate is associated with hepatotoxicity, bone marrow suppression, and potential oncologic concerns
-
Cyclosporine carries risks of nephrotoxicity, hypertension, and secondary malignancies
-
Acitretin has limited efficacy for inflammatory disease and significant teratogenicity
The finding that biologics perform no worse in terms of cancer progression or recurrence challenges long-held assumptions and encourages a more nuanced, individualized approach to treatment selection.
Implications for Clinical Practice
These findings have important implications for dermatologists, oncologists, and multidisciplinary care teams:
-
Biologics may be considered viable options for psoriasis patients with active or recent cancer when disease severity warrants systemic therapy.
-
Treatment decisions should be individualized, taking into account cancer type, stage, prognosis, and patient preferences.
-
Collaboration with oncology specialists remains essential to ensure coordinated and safe care.
-
Quality of life considerations should not be overlooked, as uncontrolled psoriasis can significantly worsen physical and psychological well-being.
Remaining Gaps and Future Directions
Despite encouraging data, several unanswered questions remain:
-
Are certain biologic classes safer than others in specific cancer types?
-
What is the optimal timing of biologic initiation following cancer treatment?
-
How do long-term outcomes compare across different malignancies?
Ongoing registry studies and long-term real-world data will be critical in refining guidelines and providing more precise risk stratification.
Conclusion
Emerging evidence suggests that biologic therapies are not associated with higher cancer progression or recurrence rates compared with conventional systemic agents in patients with psoriasis who have active cancer or a recent history of malignancy. These findings challenge longstanding clinical hesitations and support a more flexible, patient-centered approach to psoriasis management.
While caution and multidisciplinary collaboration remain essential, biologics may offer a safe and effective treatment option for a population that has historically faced limited choices. As the evidence base continues to grow, biologic therapies are likely to play an increasingly important role in the care of psoriasis patients with complex oncologic histories.
News in the same category


Daily Step Counts Combined With Genetic Risk Can Better Predict Type 2 Diabetes

Gestational Diabetes Rates Surge Across the United States

Why Does Lung Cancer Affect Non-Smokers? A Hidden Culprit in the Kitchen That Many People Overlook
6 Foods You Absolutely Need To Avoid If You Suffer From a Thyroid Disorder

Gastroenterologist says this is the #1 drink for gut health

Top 5 drinks to INSTANTLY improve leg circulation and blood flow

Five Morning Habits That May Quietly Increase Cancer Risk

Natural Home Remedies for Cough and Sore Throat
People with weak kidneys often do these 4 things every day: If you don't stop soon, it can easily damage your kidneys

I spent a couple of nights at my friend’s previous apartment and saw these unusual bumps

Understanding the Link Between Your Blood Type and Health

10 Unusual Signs Your Blood Sugar Is Constantly Too High

Five Simple Drinks That Help Eliminate Uric Acid and Prevent Gout Flare-Ups
Red and Processed Meat Consumption Increases Cancer Risk, Experts Warn

The Hidden Dangers of Eating Leftover Food Stored Overnight
Two Rare Neurologic Disorders Added to US Newborn Screening Panel

Intensive Long-Distance Running and Colon Health: Emerging Evidence of Increased Risk for Advanced Adenomas

After Many Years of Practice, Doctors Noticed Six Common Morning Habits Among Cancer Patients

Six Foods That May Help Prevent Colorectal Cancer — Especially After Age 45
News Post

16 Warning Signs of Poor Blood Circulation and How to Treat It

The Best Home Remedies For Getting Rid of Ear Infection

A Simple Act of Kindness That Turned a Lifelong Dream into Reality

Soap Left on Plates? British Dishwashing Method Sparks International Debate

A Hero on Four Paws: How a Cat’s Instincts Saved a Baby from an Alligator

Florida’s Trooper’s Law: A Landmark Step Toward Protecting Pets During Natural Disasters

An 11,000-Year-Old Indigenous Settlement in Saskatchewan Is Transforming Our Understanding of North America’s Ancient Past

Never realized this

When Speed Saves Lives: The Lamborghini Mission That Delivered Hope

Daily Step Counts Combined With Genetic Risk Can Better Predict Type 2 Diabetes

Gestational Diabetes Rates Surge Across the United States

Why Does Lung Cancer Affect Non-Smokers? A Hidden Culprit in the Kitchen That Many People Overlook
Love, Sacrifice, and the Healing Power of Commitment 💖🩺

Figo’s Bravery: A Testament to the Selflessness of Dogs 🐕💛

Braving the Storm: A Mail Carrier’s Act of Compassion ❄️💙

Belgian Prodigy Earns PhD in Quantum Physics at Just 15 🌟⚛️
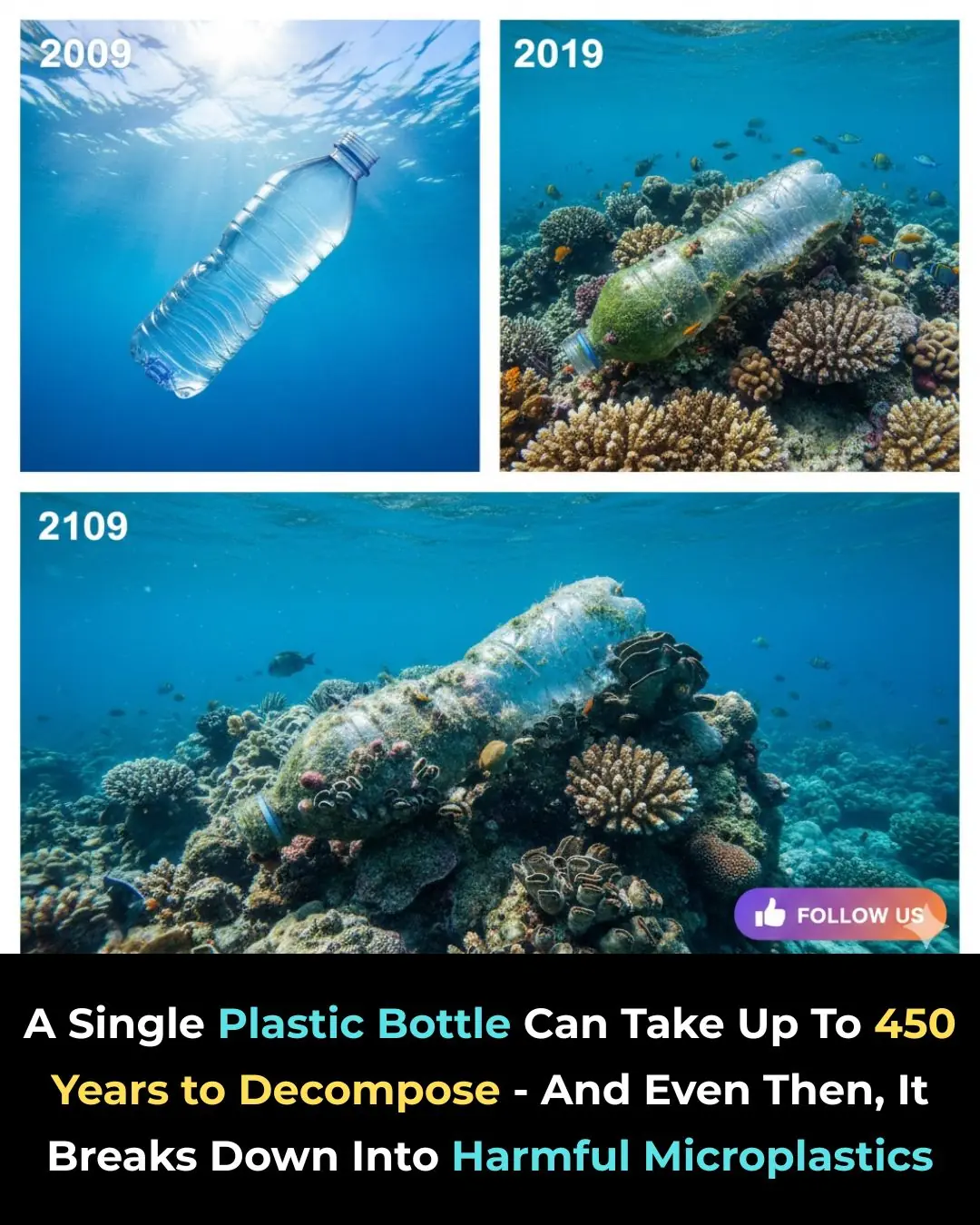
One Plastic Bottle. One Huge Problem. 🌍♻️

A Major Shake‑Up in the EV World: BYD Surpasses Tesla 🚗⚡🔋🌍

MS Treatment Costs in the United States Surge by 125% Over Two Decades