Breaking Through the Stigma as Access to GLP-1 Receptor Agonists Expands

As GLP-1 receptor agonists move into wider use for the treatment of type 2 diabetes and obesity, primary care clinicians are increasingly recognizing that prescribing these medications is only part of the challenge. Equally important—and often more complex—is the conversation that surrounds their use.
With growing public awareness, media attention, and demand for GLP-1 therapies, clinicians are navigating not only clinical decision-making but also deeply rooted stigma around weight, metabolism, and medication-assisted care. Experts say that how these conversations are framed at the primary care level can significantly influence patient trust, adherence, and long-term outcomes.
Beyond the Prescription: The Communication Gap
GLP-1 receptor agonists have demonstrated robust efficacy in improving glycemic control, promoting clinically meaningful weight loss, and reducing cardiometabolic risk. Yet many patients remain hesitant, confused, or conflicted when the topic is raised.
According to weight management specialists, patients often come to appointments with preconceived notions shaped by social media narratives, celebrity endorsements, and misinformation. Some worry that GLP-1s represent a “shortcut,” a failure of willpower, or a cosmetic rather than medical intervention.
For clinicians, addressing these concerns requires a deliberate shift away from transactional prescribing toward empathetic, patient-centered dialogue.
“Patients don’t just want to know how the drug works,” experts note. “They want to know what it says about them.”
Reframing Obesity as a Chronic Disease
One of the most effective ways to reduce stigma, clinicians say, is to consistently frame obesity as a chronic, relapsing, biologically driven disease, rather than a personal failing.
By explaining the roles of genetics, hormones, appetite regulation, and metabolic adaptation, clinicians can help patients understand why lifestyle changes alone may not produce sustained results—and why pharmacotherapy is a legitimate, evidence-based option.
This reframing also helps normalize GLP-1s alongside medications used for hypertension, dyslipidemia, or diabetes, reinforcing the idea that treating obesity medically is no different from treating any other chronic condition.
The Importance of Tone and Language
Subtle changes in language can have a powerful impact on how patients perceive GLP-1 therapy. Weight management experts emphasize avoiding terms that imply blame, moral judgment, or failure.
For example:
-
Replacing “You haven’t lost enough weight” with “Your body may be defending a higher set point”
-
Avoiding phrases like “last resort” or “extreme option”
-
Using neutral, respectful language when discussing weight and BMI
These adjustments can foster a more collaborative atmosphere and reduce patient defensiveness.
Setting Expectations and Addressing Concerns Early
Another common barrier to adherence is unrealistic expectations. Patients may expect rapid, effortless weight loss or underestimate the importance of dose titration, side-effect management, and long-term use.
Experts recommend discussing:
-
The gradual nature of dose escalation
-
Common gastrointestinal side effects and how to manage them
-
The likelihood that treatment may be long-term rather than temporary
-
The importance of continued nutrition, physical activity, and follow-up
When expectations are aligned early, patients are less likely to discontinue therapy prematurely.
Follow-Up as a Trust-Building Tool
Regular follow-up is not just a clinical necessity—it is a signal of partnership. Clinicians who schedule early check-ins after initiating GLP-1 therapy report higher adherence and greater patient satisfaction.
Follow-up visits provide opportunities to:
-
Normalize side effects
-
Reinforce progress beyond the scale, such as improved energy or glycemic control
-
Adjust dosing based on individual response
-
Revisit goals and concerns as they evolve
Patients who feel supported are more likely to remain engaged and transparent about challenges.
Addressing Cost, Access, and Equity
Stigma is also intertwined with issues of access and affordability. Insurance coverage remains inconsistent, and out-of-pocket costs can be prohibitive for many patients.
Experts caution that dismissing patient concerns about cost—or assuming financial barriers are a personal choice—can further erode trust. Transparent discussions about coverage, alternatives, and advocacy options are essential components of ethical prescribing.
A Cultural Shift in Primary Care
As GLP-1 receptor agonists become more integrated into routine care, clinicians are helping drive a broader cultural shift in how obesity and metabolic disease are perceived and treated.
Breaking through stigma requires more than clinical evidence—it requires intentional communication, humility, and respect. When clinicians take the time to listen, educate, and partner with patients, GLP-1 therapies can become not just medications, but tools for empowerment and long-term health.
Conclusion
The expansion of GLP-1 receptor agonist use represents a major advance in metabolic medicine, but its success in real-world settings depends heavily on the quality of clinician-patient conversations. By reframing obesity, refining language, setting realistic expectations, and prioritizing follow-up, primary care clinicians can help dismantle stigma and improve outcomes for patients seeking effective, compassionate care.
As experts emphasize, the prescription may start the journey—but the conversation determines where it leads.
News in the same category
From Casual Drinking to Dependence: A Recovering Alcoholic Reveals Seven Warning Signs of Addiction

Why Americans Were Shocked by the British Way of Washing Dishes
Can You Spot It? The Viral “Sniper Vision” Challenge That’s Testing Human Perception

How Japan Preserves Nature by Relocating Trees Instead of Cutting Them Down

A Simple Act of Kindness That Turned a Lifelong Dream into Reality

A Hero on Four Paws: How a Cat’s Instincts Saved a Baby from an Alligator

Florida’s Trooper’s Law: A Landmark Step Toward Protecting Pets During Natural Disasters

An 11,000-Year-Old Indigenous Settlement in Saskatchewan Is Transforming Our Understanding of North America’s Ancient Past

When Speed Saves Lives: The Lamborghini Mission That Delivered Hope

MS Treatment Costs in the United States Surge by 125% Over Two Decades

Quick thinking action by hero father saved ten lives in Swiss fire after call from daughter
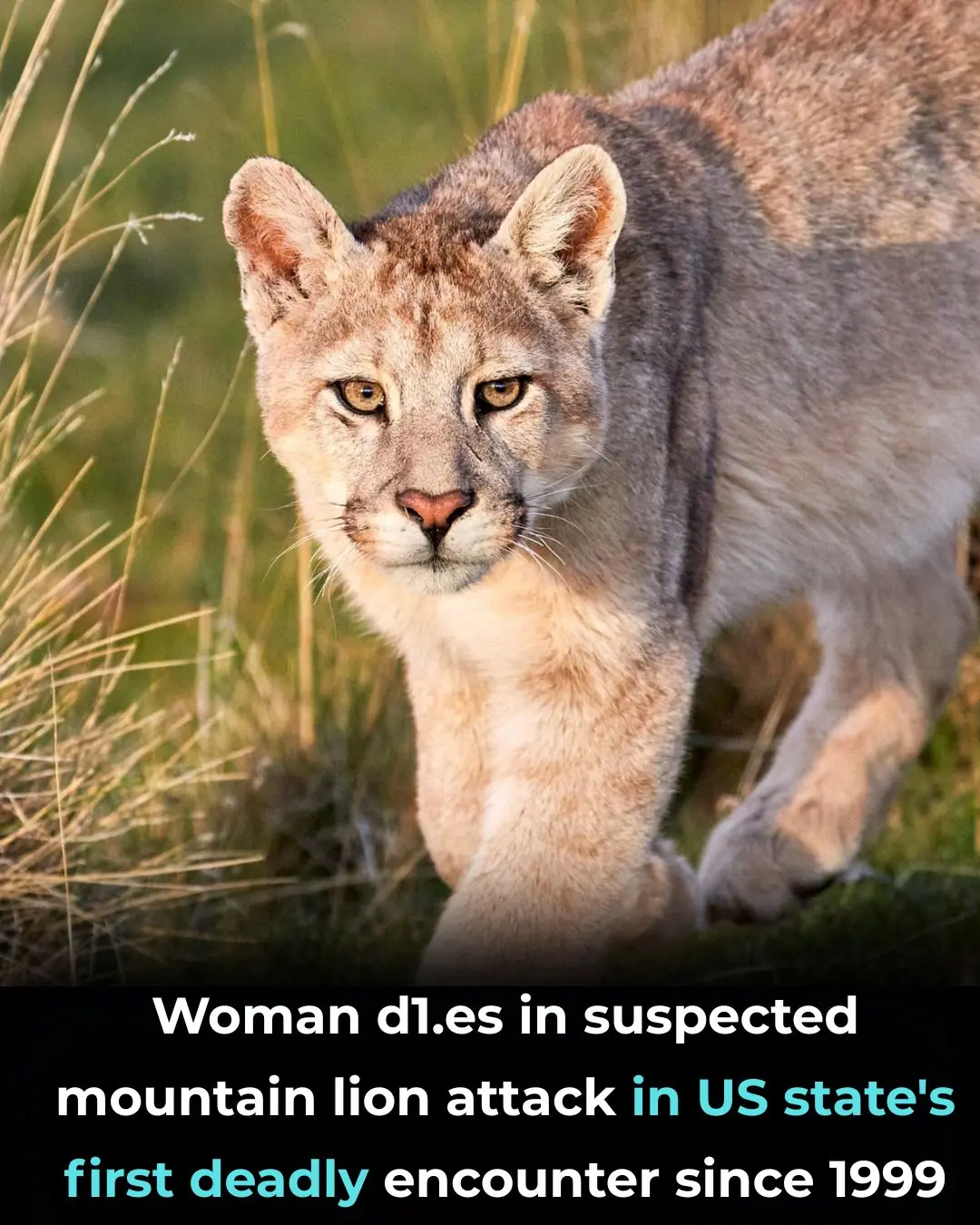
Woman d!es in suspected mountain lion attack in US state's first deadly encounter since 1999

DOJ fails again to get grand jury to indict New York AG Letitia James, a Trump target
North Dakota Little Caesars Goes Viral for Inviting Hungry Strangers Inside After Trash Can Incident
Jeff Bezos Warns Earth Has No Plan B, Calls for Moving Heavy Industry Into Space

South Florida Lifeguard Declines Job Offer After Rescue Controversy

Joe Budden Says He Feels Diddy 'Didn't Get Enough Time' in Prison After Watching Netflix Doc

GRAMMY-Winning Star Jekalyn Carr Sells Out First Signature Doll in One Hour

NBA Great Allen Iverson Backed an Affordable Housing Project in Virginia — And It's Moving Forward
News Post
Fears of a Texas Serial Killer Intensify After Three More Bodies Are Recovered from Houston Bayous
From Casual Drinking to Dependence: A Recovering Alcoholic Reveals Seven Warning Signs of Addiction

Why Americans Were Shocked by the British Way of Washing Dishes

No one told me
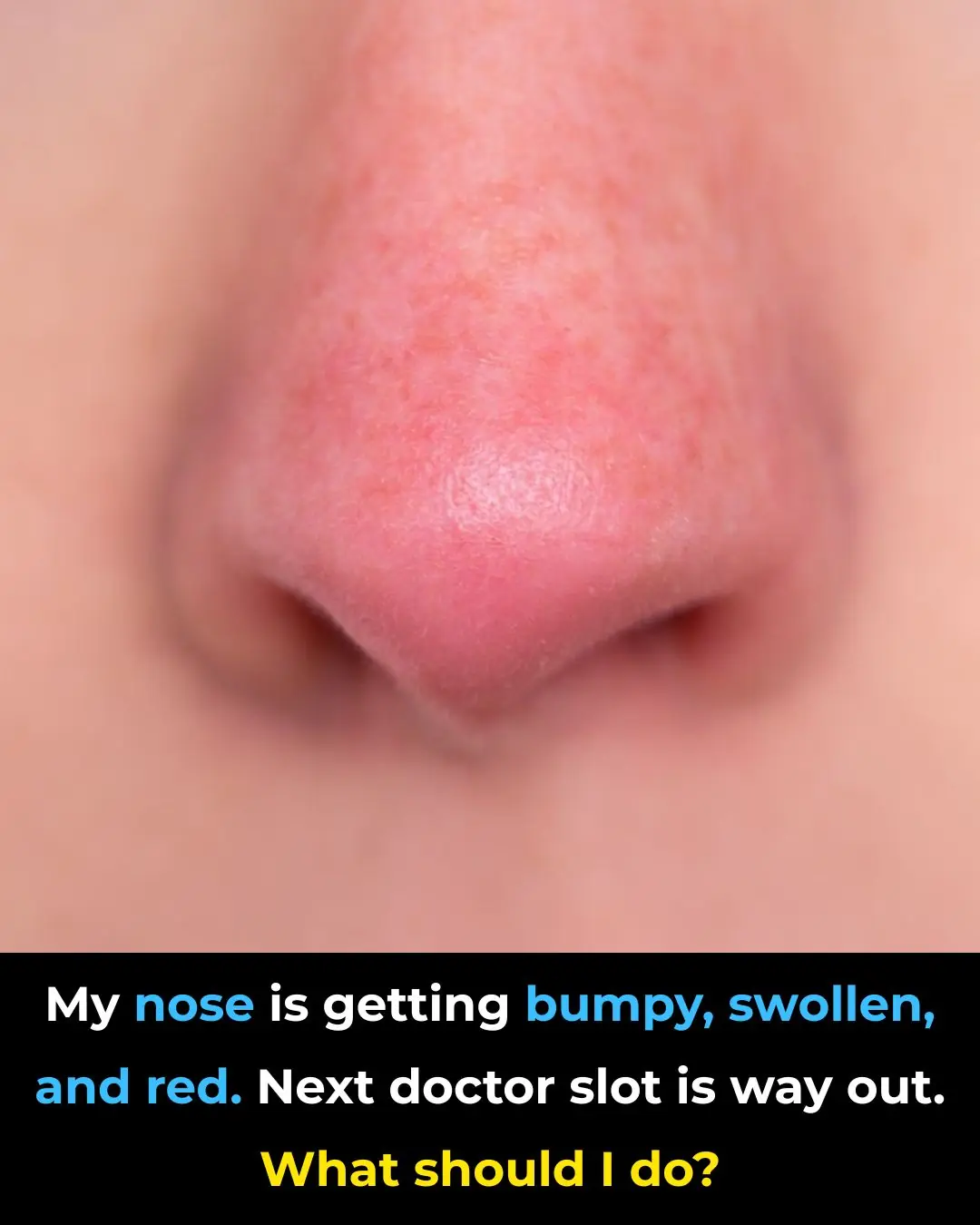
My nose is getting bumpy, swollen, and red. Next doctor slot is way out. What should I do?
Can You Spot It? The Viral “Sniper Vision” Challenge That’s Testing Human Perception

Most Doctors Won’t Tell You, But This Can Cut Heart Attack & Stroke Risk By 80%

The Best Proven Ways to Heal Scars Naturally (Evidence Based)

How Japan Preserves Nature by Relocating Trees Instead of Cutting Them Down

16 Warning Signs of Poor Blood Circulation and How to Treat It

The Best Home Remedies For Getting Rid of Ear Infection

A Simple Act of Kindness That Turned a Lifelong Dream into Reality

Soap Left on Plates? British Dishwashing Method Sparks International Debate

A Hero on Four Paws: How a Cat’s Instincts Saved a Baby from an Alligator

Florida’s Trooper’s Law: A Landmark Step Toward Protecting Pets During Natural Disasters

An 11,000-Year-Old Indigenous Settlement in Saskatchewan Is Transforming Our Understanding of North America’s Ancient Past

Never realized this

When Speed Saves Lives: The Lamborghini Mission That Delivered Hope

Daily Step Counts Combined With Genetic Risk Can Better Predict Type 2 Diabetes
