Can Relative Fat Mass Replace BMI in Assessing Obesity?

For decades, body mass index (BMI) has been the dominant tool used to define and diagnose obesity. Simple, inexpensive, and easy to calculate, BMI has become deeply embedded in clinical practice, public health guidelines, insurance policies, and research. Yet its limitations have long been acknowledged. Now, a growing body of evidence—and a landmark report from The Lancet Commission—suggests that relying on BMI alone may do more harm than good.
Why BMI Falls Short
BMI is calculated using only height and weight. It does not distinguish between fat mass and lean muscle, nor does it capture fat distribution or metabolic health. As a result, individuals with high muscle mass may be mislabeled as obese, while others with normal BMI but high body fat—particularly visceral fat—may go undiagnosed despite elevated health risks.
This oversimplification has real clinical consequences. BMI alone cannot determine whether excess body fat is causing organ dysfunction, physical limitation, or metabolic disease. Yet these are precisely the factors that define obesity as a medical condition rather than a numerical category.
The Lancet Commission’s Call for Change
Recognizing these shortcomings, The Lancet Commission on Clinical Obesity concluded that BMI alone is insufficient to diagnose obesity as a disease. The Commission recommended a more comprehensive diagnostic framework that incorporates:
-
Additional body composition measurements (such as waist circumference or relative fat mass)
-
Evidence of organ dysfunction (cardiovascular, metabolic, respiratory, or musculoskeletal)
-
Functional limitations that impair daily life or quality of living
This shift reframes obesity not merely as excess weight, but as a condition defined by excess adiposity that causes harm to health and function.
What Is Relative Fat Mass?
Relative fat mass (RFM) is an emerging metric that estimates body fat percentage using height and waist circumference rather than weight. Unlike BMI, RFM better reflects central adiposity, which is more strongly associated with cardiometabolic risk.
Studies suggest that RFM correlates more closely with actual body fat percentage and may offer improved accuracy across sexes, age groups, and ethnicities. While not perfect, it represents a meaningful step toward more precise obesity assessment.
Benefits of Moving Beyond BMI
Adopting a broader diagnostic approach could bring multiple benefits:
Preventing misdirected treatment
Patients would be less likely to receive unnecessary interventions based solely on BMI, and more likely to receive care when excess fat truly affects health.
Reducing healthcare costs
By targeting treatment to those with clinically significant obesity, health systems could avoid overtreatment and allocate resources more efficiently.
Reducing stigma
BMI-based labels often contribute to weight stigma, shame, and discrimination. A functional, health-based definition shifts the focus from appearance to well-being.
Improving access to appropriate care
Patients who experience obesity-related complications but fall below BMI cutoffs could finally qualify for treatment, while others may avoid being incorrectly medicalized.
Challenges and the Path Forward
Despite its advantages, replacing BMI entirely will not be easy. BMI remains deeply ingrained in clinical workflows and population-level surveillance. New tools must be validated, standardized, and made accessible across healthcare settings.
The future may not lie in choosing a single replacement for BMI, but in using BMI as an initial screening tool—followed by more precise assessments of fat distribution, metabolic health, and functional impact.
Redefining Obesity as a Disease
Ultimately, the Lancet Commission’s message is clear: obesity should be diagnosed based on health consequences, not numbers alone. By integrating body composition measures like relative fat mass with clinical evidence of dysfunction, medicine can move toward a more accurate, compassionate, and effective approach to obesity care.
Shifting away from BMI-centric thinking is not just a technical adjustment—it is a necessary evolution toward better science, better care, and greater respect for the complexity of human bodies.
News in the same category
Frozen Meat Rock-Hard from the Freezer? Use These Two Simple Methods to Thaw It Quickly Without Waiting

5 Types of Eggs That Can Be Harmful If Consumed Too Often

Women Who Drink Perilla Leaf Water With Lemon at These 3 Times May Notice Brighter Skin and a Slimmer Waist
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)
How to Naturally Increase Estrogen Levels

Evidence-Based Health Benefits of Honey (Raw, Pure, Natural) + Turmeric Golden Honey Recipe
Foamy Urine: Here’s Why You Have Bubbles in Your Urine
Why Almonds Are So Good for You: Health Benefits of Almonds Backed by Science
No Reset: When a Clinical Mindset Takes Over Your Whole Life

Dermatology Data Reinforce the Relative Safety of JAK Inhibitors
Can Cuffless Blood Pressure Devices Transform Cardiovascular Disease Prevention and Treatment?
Early-stage stomach cancer is often accompanied by these 6 symptoms

6 Things People Who Live to 100 Do Every Week to Stay Healthy

Seven Foods That Rarely Spoil: Still Safe to Eat Even After the Expiration Date

Five Parts of Fish That Are Dirty and Potentially Toxic — The First One Is Often Mistaken as Healthy but Can Be Fatal

Health Benefits of Boiled Green Bananas

How to Drink Lemon Turmeric Water in the Morning to Support Liver and Kidney Detox Without Harming the Stomach
When Women Target Other Women: The Hidden Wounds of Bullying in Medicine
News Post
Simple Tips to Store Ginger Without a Refrigerator: Keep It Fresh for a Year Without Sprouting or Spoiling
Frozen Meat Rock-Hard from the Freezer? Use These Two Simple Methods to Thaw It Quickly Without Waiting

5 Types of Eggs That Can Be Harmful If Consumed Too Often

Women Who Drink Perilla Leaf Water With Lemon at These 3 Times May Notice Brighter Skin and a Slimmer Waist

Tata Sierra vs Mahindra XUV 7XO: A Mid‑Size SUV Showdown 🚙🔥

This red, scaly patch won’t go away. It's all over my forehead and doctor isn't answering me. What is it?
I keep wondering why this happens to me
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)
How to Naturally Increase Estrogen Levels

Evidence-Based Health Benefits of Honey (Raw, Pure, Natural) + Turmeric Golden Honey Recipe
Foamy Urine: Here’s Why You Have Bubbles in Your Urine
Why Almonds Are So Good for You: Health Benefits of Almonds Backed by Science
When Garlic Turns Harmful: Common Mistakes That Can Make a Healthy Food Risky
The Most Affordable Food That Supports Bone Health and Helps Fight Osteoporosis

Onion Water for Hair Growth: What It Can Do, What It Can’t, and What Science Really Says

A Cardiac Surgeon’s Warning: Why Many Elderly Patients Should Be Cautious About This Common Medication
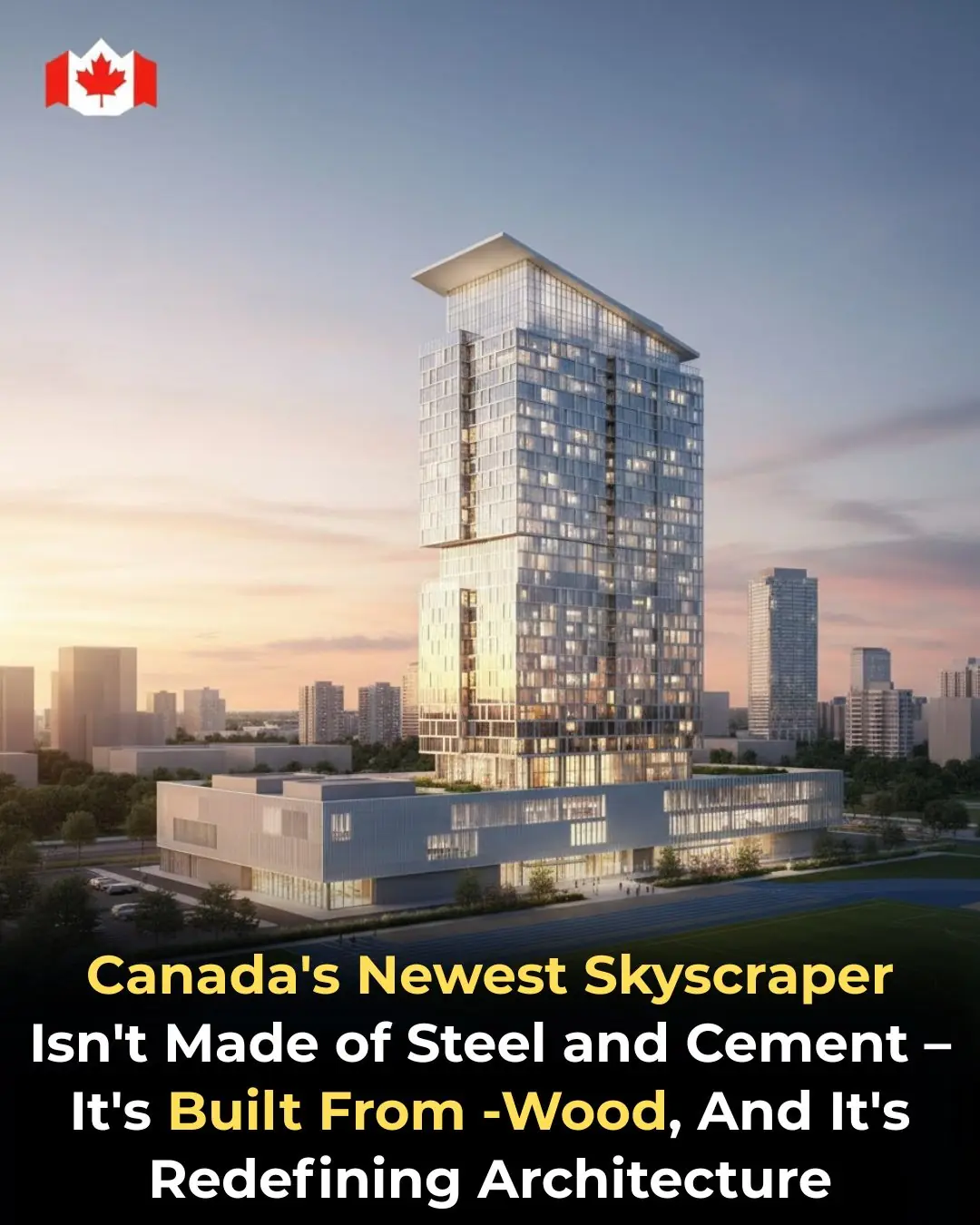
Canada Builds the Future in Wood: Inside Toronto’s Groundbreaking Timber Skyscraper

The Woman Who Refused to Quit: How Jacklyn Bezos Changed Her Life—and Helped Shape the Future of the World
San Francisco Establishes Reparations Fund Framework to Address Historical Racial Inequities
