This red, scaly patch won’t go away. It's all over my forehead and doctor isn't answering me. What is it?
Noticing a red, scaly patch on your forehead that doesn’t seem to heal can be unsettling. When it lingers for weeks or even months, it’s natural to feel worried—especially if you can’t get immediate answers from a doctor. While not every stubborn skin patch is dangerous, understanding the possible causes is essential for both your peace of mind and your long-term skin health.
One possible explanation for a persistent, rough patch on sun-exposed skin is actinic keratosis, a common but often misunderstood condition. Although it may initially appear harmless, actinic keratosis deserves attention because, in some cases, it can progress into a more serious form of skin cancer. This article explores what actinic keratosis is, how to recognize it, what causes it, and what steps you should take if you suspect you may have it.
1. What Is Actinic Keratosis?
Actinic keratosis—also called solar keratosis—is a skin condition caused by long-term exposure to ultraviolet (UV) radiation. It develops gradually, often after years of sun exposure, and is considered precancerous because it has the potential to evolve into squamous cell carcinoma.
These lesions typically appear on areas of the body that receive the most sun, such as the forehead, face, ears, scalp, neck, chest, forearms, hands, and lips. Actinic keratoses often feel rough or sandpaper-like and may be easier to feel than see at first.
They usually present as small, scaly patches that range in color from flesh-toned to red or brown. While many are painless, some can itch, sting, or become tender, especially when rubbed or exposed to sunlight.
2. Recognizing the Symptoms
The hallmark sign of actinic keratosis is a dry, rough, or scaly patch of skin, generally less than one inch (2.5 cm) in diameter. These patches may be flat or slightly raised and can vary in appearance over time.
Additional symptoms may include:
-
Mild itching or burning
-
A prickling or tingling sensation
-
Inflammation or redness
-
Occasional bleeding or crusting
Because actinic keratosis can resemble other skin conditions—such as eczema, psoriasis, or simple sun damage—professional evaluation is crucial for an accurate diagnosis.
3. Causes and Risk Factors
The primary cause of actinic keratosis is cumulative UV exposure from sunlight or tanning beds. The risk increases with age, as sun damage builds up over many years rather than occurring all at once.
People at higher risk include:
-
Individuals with fair or light skin
-
Those with blue or green eyes and blond or red hair
-
People who live in sunny or high-altitude regions
-
Individuals with weakened immune systems
-
Anyone with a personal or family history of skin cancer
Frequent sunburns earlier in life significantly increase the likelihood of developing actinic keratosis later on.
4. How Sun Exposure Damages the Skin
Ultraviolet radiation penetrates the skin and damages the DNA within skin cells. Over time, this damage interferes with normal cell repair and regeneration, leading to abnormal growth patterns.
Chronic sun exposure contributes not only to actinic keratosis but also to:
-
Premature skin aging
-
Wrinkles and fine lines
-
Sunspots and discoloration
-
Increased risk of skin cancers
This makes sun protection one of the most important preventive measures you can take for your skin.
5. When You Should See a Doctor
Any skin lesion that does not heal, continues to grow, or changes in color or texture should be evaluated by a healthcare professional. Early detection of actinic keratosis greatly reduces the risk of complications.
Seek medical advice promptly if the patch:
-
Becomes painful or itchy
-
Bleeds or crusts repeatedly
-
Changes rapidly in appearance
-
Spreads or multiplies
A dermatologist can confirm the diagnosis and recommend appropriate treatment.
6. Treatment Options Available
Treatment depends on the size, location, and number of lesions. Common medical treatments include:
-
Cryotherapy: Freezing the lesion with liquid nitrogen
-
Topical medications: Such as 5-fluorouracil, imiquimod, or diclofenac
-
Photodynamic therapy: Using light to activate a photosensitive medication
-
Surgical removal: In cases where lesions are thick or suspicious
Most treatments are highly effective when actinic keratosis is caught early.
7. Home Remedies and Internet “Hacks”: Proceed with Caution
You may find online claims promoting home remedies like apple cider vinegar, coconut oil, or aloe vera. While these substances may soothe the skin, there is little scientific evidence that they can treat actinic keratosis effectively.
Relying on unproven remedies can delay proper medical care and increase the risk of progression. Always consult a healthcare provider before attempting any home-based treatment.
8. Why Regular Skin Exams Matter
Routine skin examinations are essential for detecting actinic keratosis and other skin abnormalities early. Dermatologists can identify lesions that you may overlook and monitor changes over time.
Annual skin checks are especially important if you:
-
Have a history of sun exposure
-
Have fair or sensitive skin
-
Have had actinic keratosis or skin cancer before
Early intervention leads to better outcomes and fewer complications.
9. Protecting Your Skin Going Forward
Preventing further sun damage is key to stopping new lesions from forming. Protective strategies include:
-
Using broad-spectrum sunscreen (SPF 30 or higher) daily
-
Reapplying sunscreen every two hours outdoors
-
Wearing hats, sunglasses, and protective clothing
-
Seeking shade during peak sun hours
-
Avoiding tanning beds entirely
Consistent sun protection can significantly reduce future risk.
10. What If Your Doctor Is Unavailable?
If you’re unable to reach your regular doctor, consider scheduling a telemedicine consultation with a dermatologist. Many skin conditions, including actinic keratosis, can be initially evaluated through photos or video visits.
In the meantime, keep track of any changes in the lesion’s size, color, or symptoms. If you notice signs of infection, severe pain, or rapid growth, seek urgent medical care.
11. Long-Term Outlook and Prevention
With early diagnosis and proper treatment, the outlook for actinic keratosis is generally very good. However, because sun damage accumulates over time, new lesions may continue to appear.
Long-term prevention focuses on:
-
Ongoing sun protection
-
Regular skin screenings
-
Early treatment of new lesions
By staying proactive, you can protect your skin and reduce the risk of more serious conditions in the future.
News in the same category

I keep wondering why this happens to me

7 easiest ways to distinguish real milk from fake milk that consumers should know by heart

How to Restore a Worn Non-Stick Pan Instead of Throwing It Away

I keep noticing thin black lines forming above my door frames, and they seem to get darker every winter. What can I do to fix?

No one told me
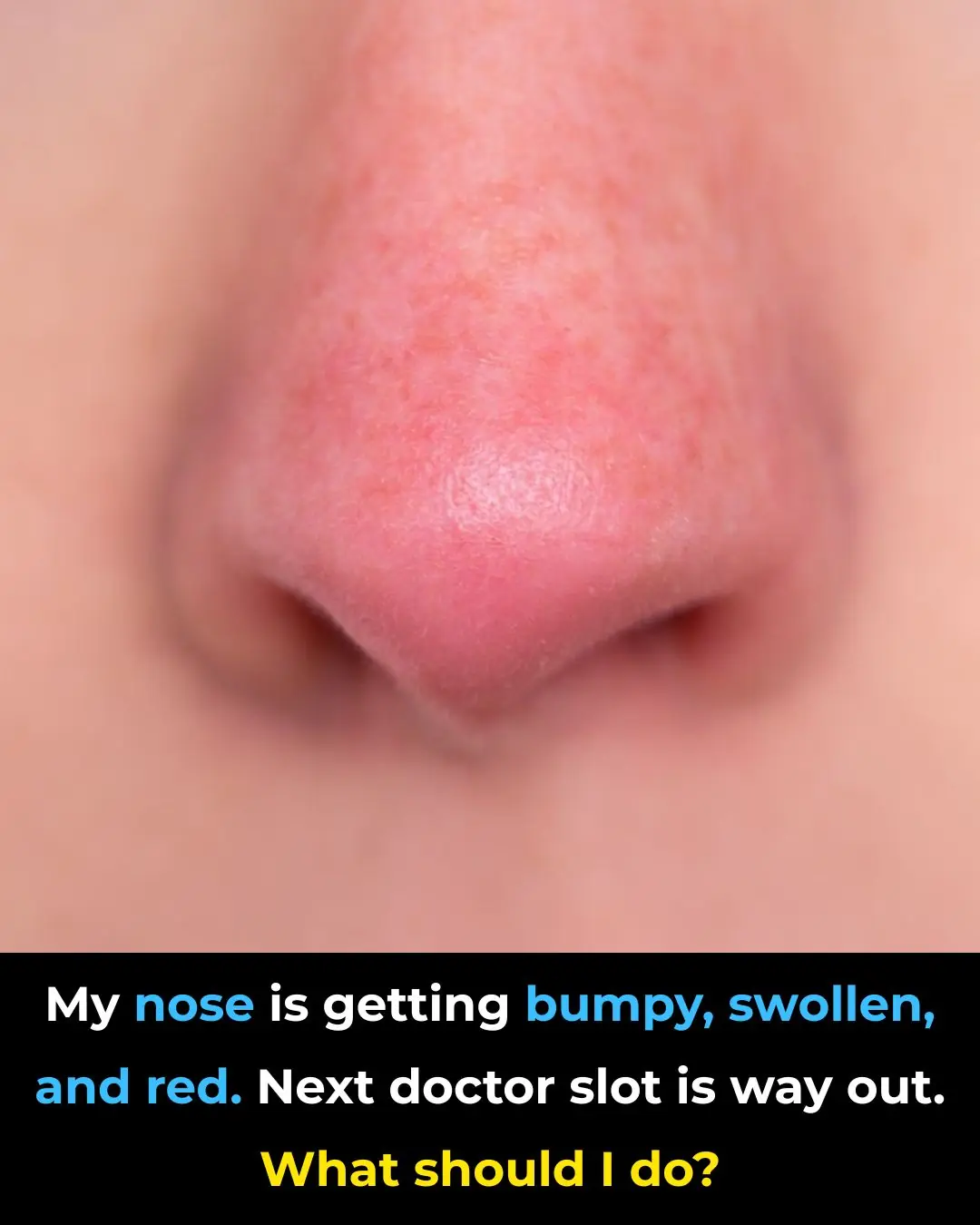
My nose is getting bumpy, swollen, and red. Next doctor slot is way out. What should I do?

Never realized this
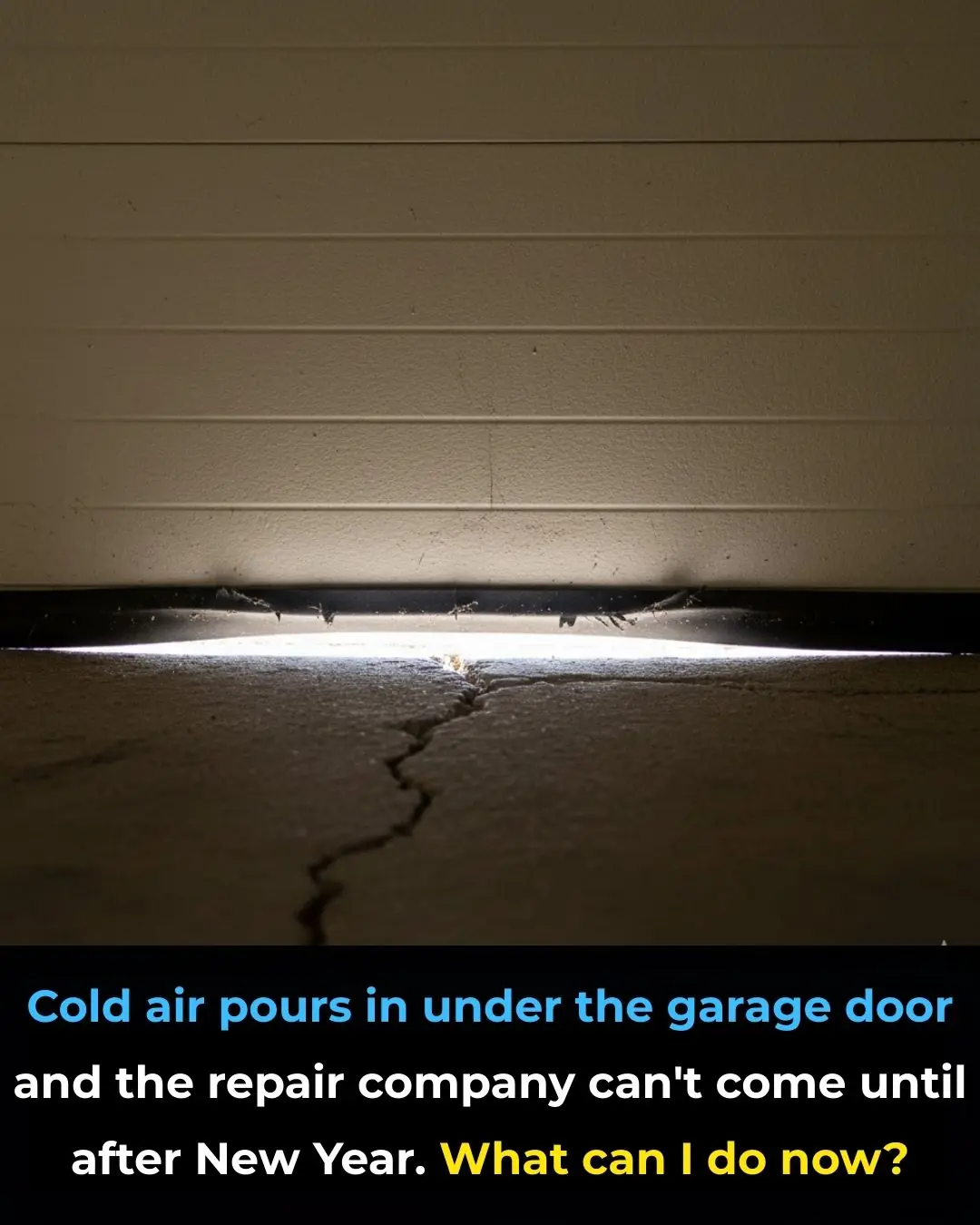
Cold air pours in under the garage door and the repair company can’t come until after New Year. What can I do now?

I swear, I didn’t have the faintest clue about this!
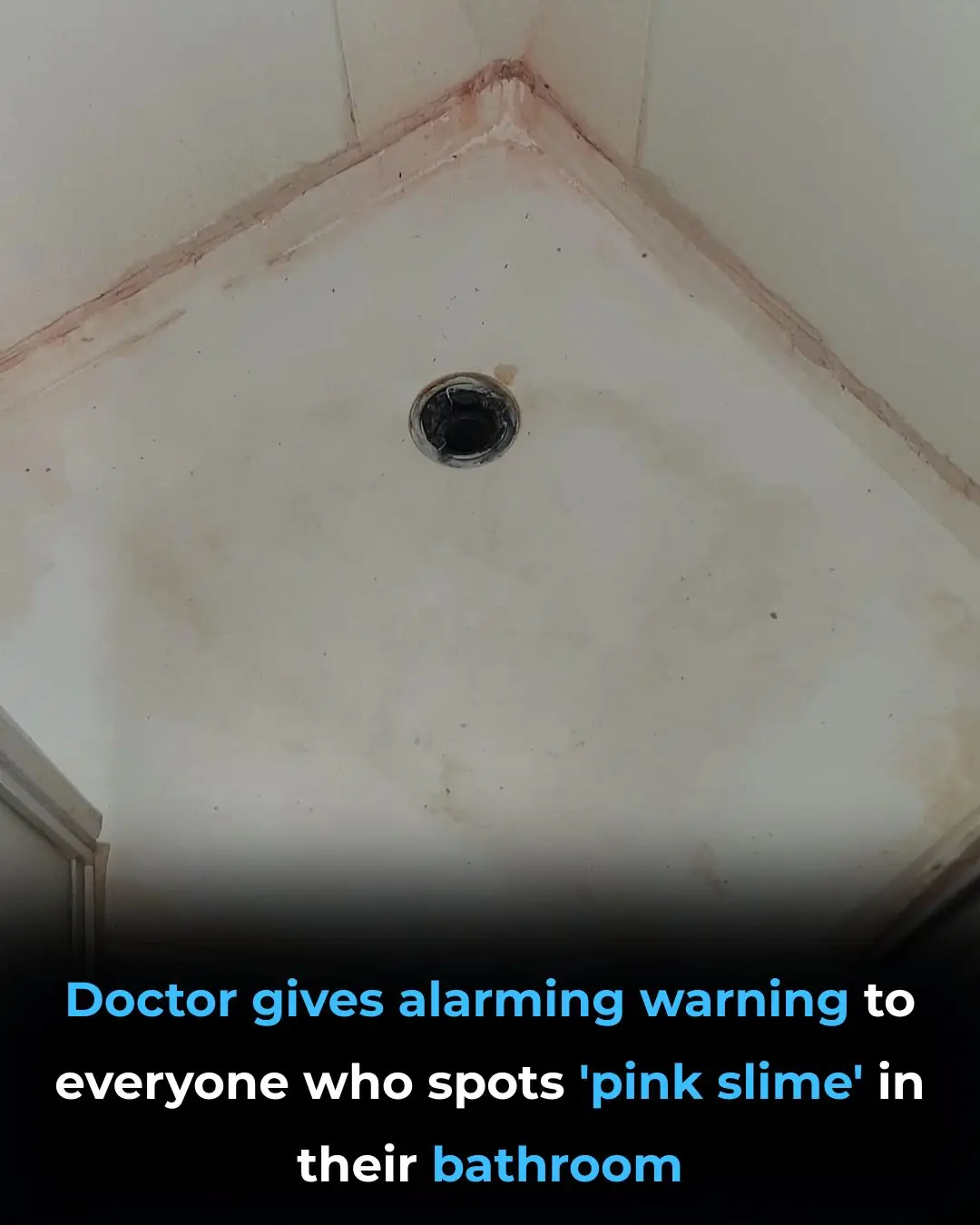
Thought this was mold but I guess not. Am gonna check my bathroom again
If you eat cucumbers everyday, this is what happens to your body

Your method isn't quite right. Here's the correct way to maintain a clean home.

Don't put the scallions straight into the refrigerator after buying them; follow this method, and they'll last for a whole month without spoiling.

Found this on my son’s scalp. Have no idea what it is and we can’t get a doc appt soon. Tips?
Cutting lemons seems simple but many people do it wrong

Most people will go their entire life without ever knowing what the little arrow next to the gas gauge actually means

3 types of fruits that are cheap in Vietnamese markets but are considered "pure gold" to protect health

Found this weird skin on my son's ear this morning. Doc appt is a week away. What can I do?
News Post

Jeezy Calls Out Industry for Exploiting Trauma in Young Rappers
Marlon Wayans warns 50 Cent

Bun B Expands Trill Burgers with New Missouri City Location

Octavia Spencer celebrates 'iconic' Sinners' duo Ryan Coogler and Michael B. Jordan for EW's 2025 Entertainers of the Year
Lil Durk's Legal Team Alleges He's Spent 131 Days in Solitary Confinement Over Apple Watch
DMX Will Posthumously Become Ordained Minister at Historic Underground Railroad Church
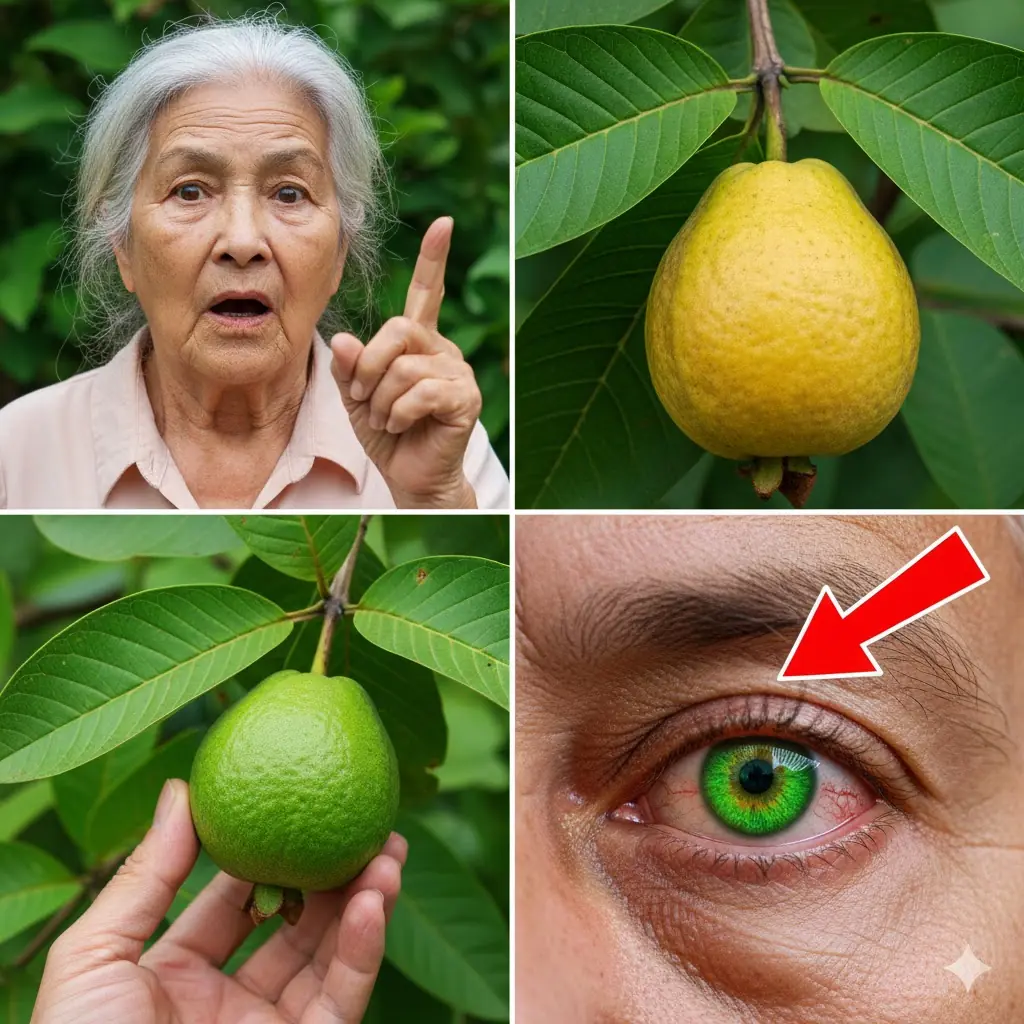
How Guava Can Naturally Support Your Eye Health: Surprising Benefits and Safe Remedies

Grape Hyacinth (Muscari): A Tiny Spring Wonder with Surprising Benefits and Uses

12 Surprising Benefits of Bull Thistle Root (And Safe Ways to Use It Naturally)
14 Little-Known Health Benefits of Moringa Leaves

Tips for preserving bean sprouts to keep them crispy and prevent them from turning black for 7 days.
Simple Tips to Store Ginger Without a Refrigerator: Keep It Fresh for a Year Without Sprouting or Spoiling
Frozen Meat Rock-Hard from the Freezer? Use These Two Simple Methods to Thaw It Quickly Without Waiting

5 Types of Eggs That Can Be Harmful If Consumed Too Often

Women Who Drink Perilla Leaf Water With Lemon at These 3 Times May Notice Brighter Skin and a Slimmer Waist

Tata Sierra vs Mahindra XUV 7XO: A Mid‑Size SUV Showdown 🚙🔥
I keep wondering why this happens to me
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)