Is Alzheimer’s Disease More Common Than Previously Thought?

Recent findings from a large population-based study suggest that Alzheimer’s disease (AD) may be more widespread in certain age groups than previously estimated. By using blood-based biomarkers rather than relying solely on clinical symptoms, researchers are gaining a clearer picture of how common Alzheimer’s pathology truly is across different stages of aging.
A New Way to Measure Alzheimer’s Risk
Traditionally, Alzheimer’s disease has been diagnosed based on cognitive symptoms, neuroimaging, and cerebrospinal fluid tests—methods that are often costly, invasive, or applied late in the disease process. In contrast, this new study used blood tests capable of detecting biomarkers associated with Alzheimer’s pathology, such as amyloid-beta and tau proteins.
Because blood testing can be applied more broadly in the general population, researchers were able to estimate the prevalence of Alzheimer’s disease across different age groups more accurately than before.
Higher Rates of Alzheimer’s Dementia in Older Adults
The study found that Alzheimer’s dementia is significantly more common in older adults than earlier estimates suggested. Among people aged 70 and older, rates of Alzheimer’s dementia were notably higher, indicating that a substantial portion of this population may already have progressed beyond the preclinical stage of the disease.
These findings reinforce the idea that Alzheimer’s disease is not a rare condition of extreme old age, but rather a widespread public health challenge that grows rapidly with aging.
Lower Preclinical Alzheimer’s in Younger Groups
Interestingly, the researchers observed lower rates of preclinical Alzheimer’s disease—defined as the presence of Alzheimer’s biomarkers without cognitive symptoms—among younger adults. This suggests that widespread early pathology may not be as common in midlife as previously feared.
However, the transition from preclinical disease to symptomatic dementia appears to accelerate later in life, underscoring the importance of monitoring cognitive health as people age.
More Than 1 in 10 Older Adults May Be Eligible for Treatment
One of the most striking findings of the study is its implication for treatment eligibility. The researchers estimated that more than 1 in 10 people over the age of 70 may meet the biological criteria for monoclonal antibody therapies designed to slow cognitive decline.
These therapies, which target amyloid pathology in the brain, have recently gained regulatory approval in several countries. While they do not cure Alzheimer’s disease, they may help slow disease progression in selected patients—particularly those diagnosed early.
Implications for Public Health and Clinical Practice
The study highlights several important implications:
-
Alzheimer’s disease may be underdiagnosed, especially in older adults who have not undergone biomarker testing.
-
Blood-based screening tools could transform early detection and population-level risk assessment.
-
Healthcare systems may face increasing demand for diagnostic services, specialist care, and disease-modifying therapies.
-
Early identification could allow more patients to benefit from treatments that slow cognitive decline rather than only managing symptoms.
Looking Ahead
As blood tests for Alzheimer’s disease become more accessible and accurate, our understanding of how common the disease truly is will continue to evolve. This study suggests that Alzheimer’s disease may affect a larger segment of the aging population than previously thought—particularly among those over 70.
Early detection, combined with emerging therapies, offers hope for changing the trajectory of Alzheimer’s disease. However, it also calls for careful planning, ethical considerations, and equitable access to testing and treatment as this new era of Alzheimer’s care unfolds.
News in the same category
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes

Surprising Health Benefits of Purslane (Portulaca oleracea)

Rising Deaths From Stomach Cancer: Doctors Warn — See These 4 Abdominal Signs and Seek Medical Care Immediately

Australia is replacing animal testing with smarter, humane science
Cracked Egg in Your Carton? Here’s When It's Safe to Eat—And When to Toss

Scientists Restore Natural Hearing Using Stem Cells in a Historic Medical Breakthrough
Morning Swelling in Kidney Disease: What Your Body Is Trying to Tell You

Cancer May Show These 2 Warning Signs at Night — Everyone Should Be Aware
Coffee Consumption May Slow Biological Aging in Severe Mental Illness

A French-made artificial heart brings new life to patients once dependent on donor transplants.
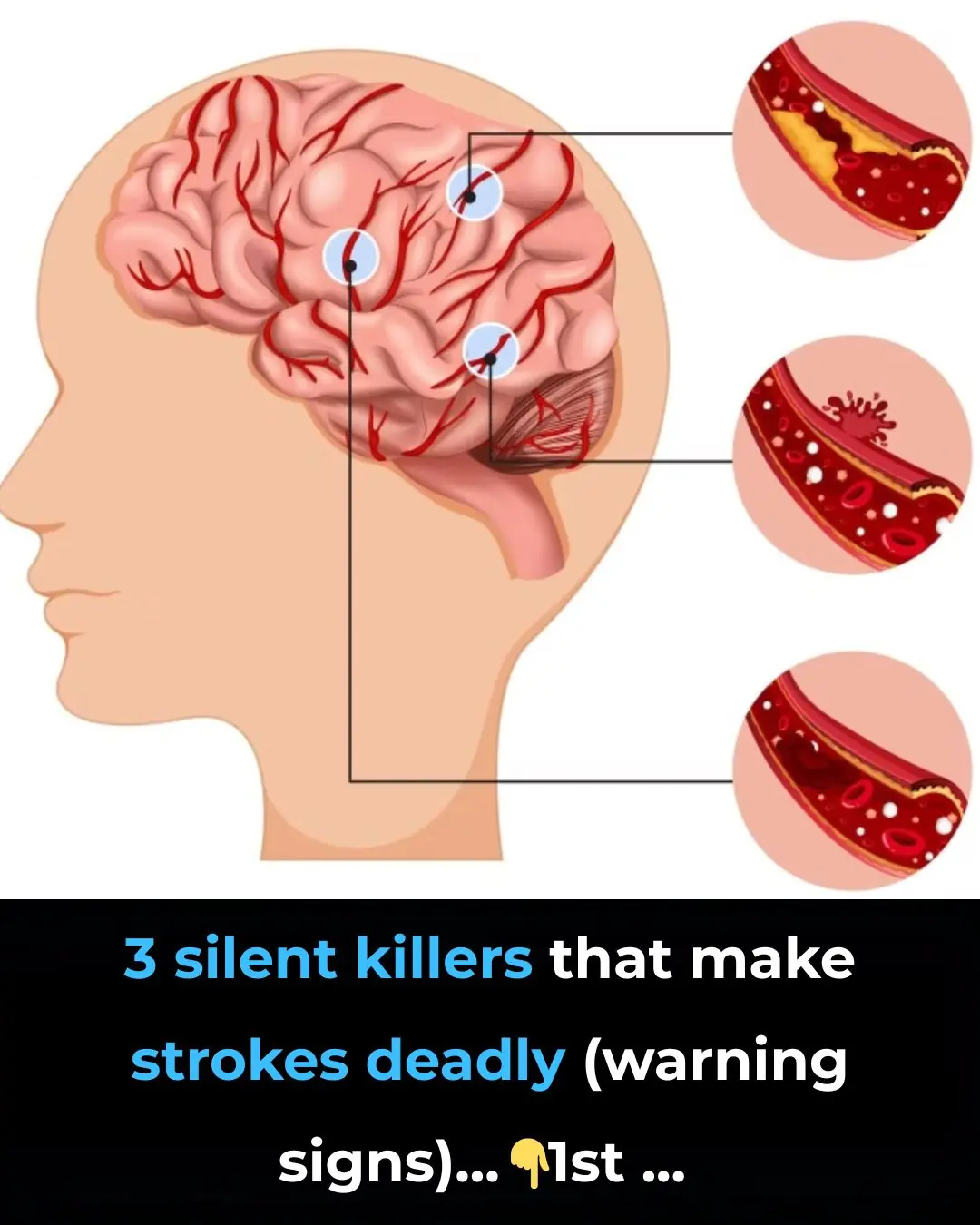
3 silent killers that make strokes deadly (warning signs)

You’d Be Surprised How Your Sleeping Environment Impacts Your Body and Mind

What To Know and Do About Pain Under Your Left Rib Cage
What Causes a Toenail To Turn Black?

7 Foods To Help You Live a Longer, Healthier Life

Why So Many Women Wake Up With Bruises They Don’t Remember Getting
News Post
Advancing Clinical Excellence in IgA Nephropathy

3 types of fruits that are cheap in Vietnamese markets but are considered "pure gold" to protect health

Found this weird skin on my son's ear this morning. Doc appt is a week away. What can I do?

My nana taught me this hack to get rid of dark circles in 5 mins with 0 work. Here’s how it works
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes
Garlic with Olive Oil Over 50: The Irreversible Body Reaction Everyone’s Talking About

Discover How Baking Soda Could Transform Your Skin’s Appearance in Minutes – Even After 70!

What Happens When You Add Just 2 Garlic Cloves a Day to Your Routine – Even After 50!

13 Subtle Signs Your Kidneys May Need Attention

Stop Shaving? Exploring Popular Home Remedies for Hair Removal

Discover the Hidden Power of Ginger Oil: Why Women Over 65 Are Seeing Thicker, Darker Hair Naturally

Top 10 Foods That May Help Reduce Frequent Nighttime Urination (Nocturia)

Why Toothpaste and Baking Soda Aren’t the Answer for Wrinkles and Dark Spots – And What Might Help Instead
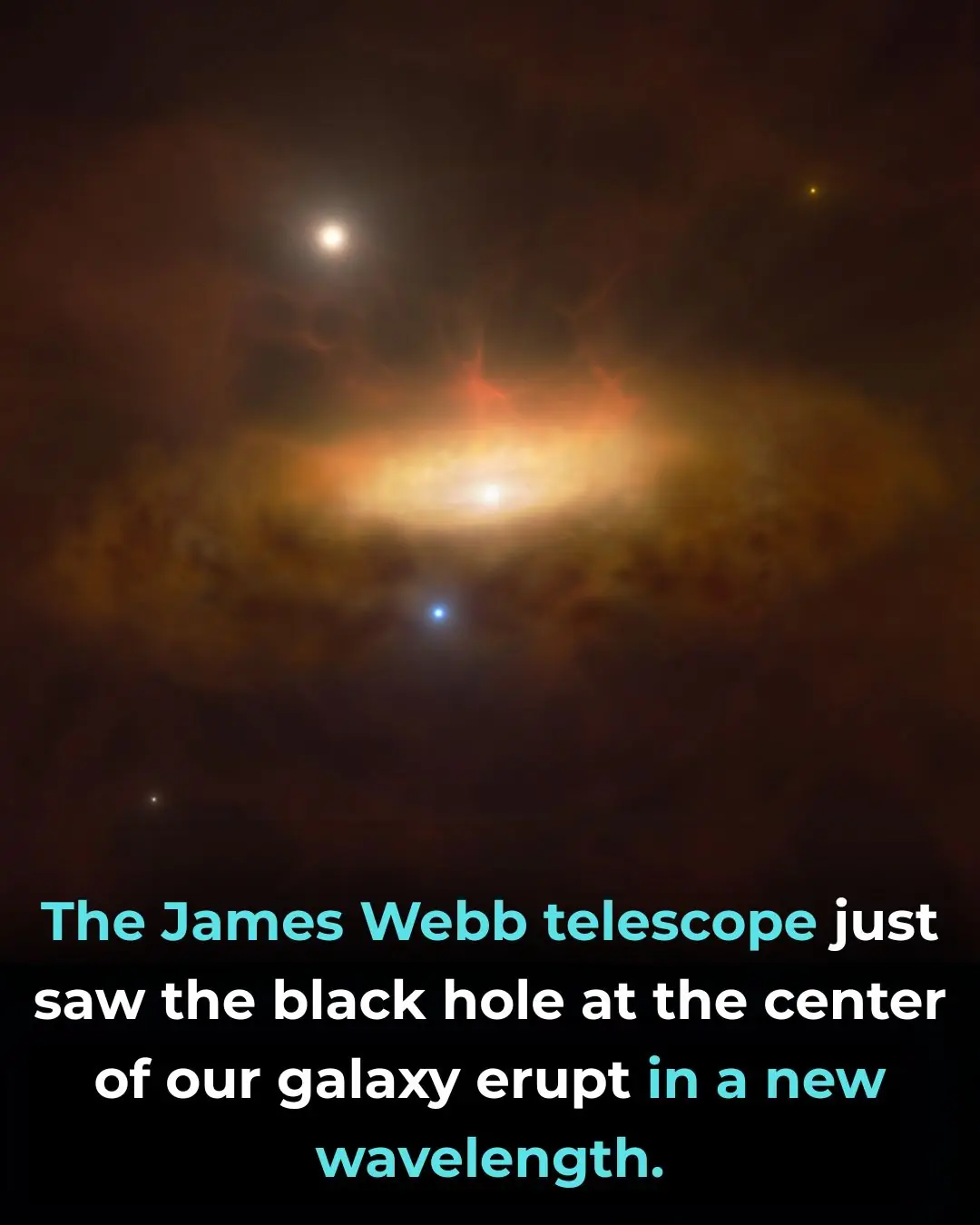
James Webb Space Telescope Reveals Hidden Mid-Infrared Flares from the Milky Way’s Central Black Hole
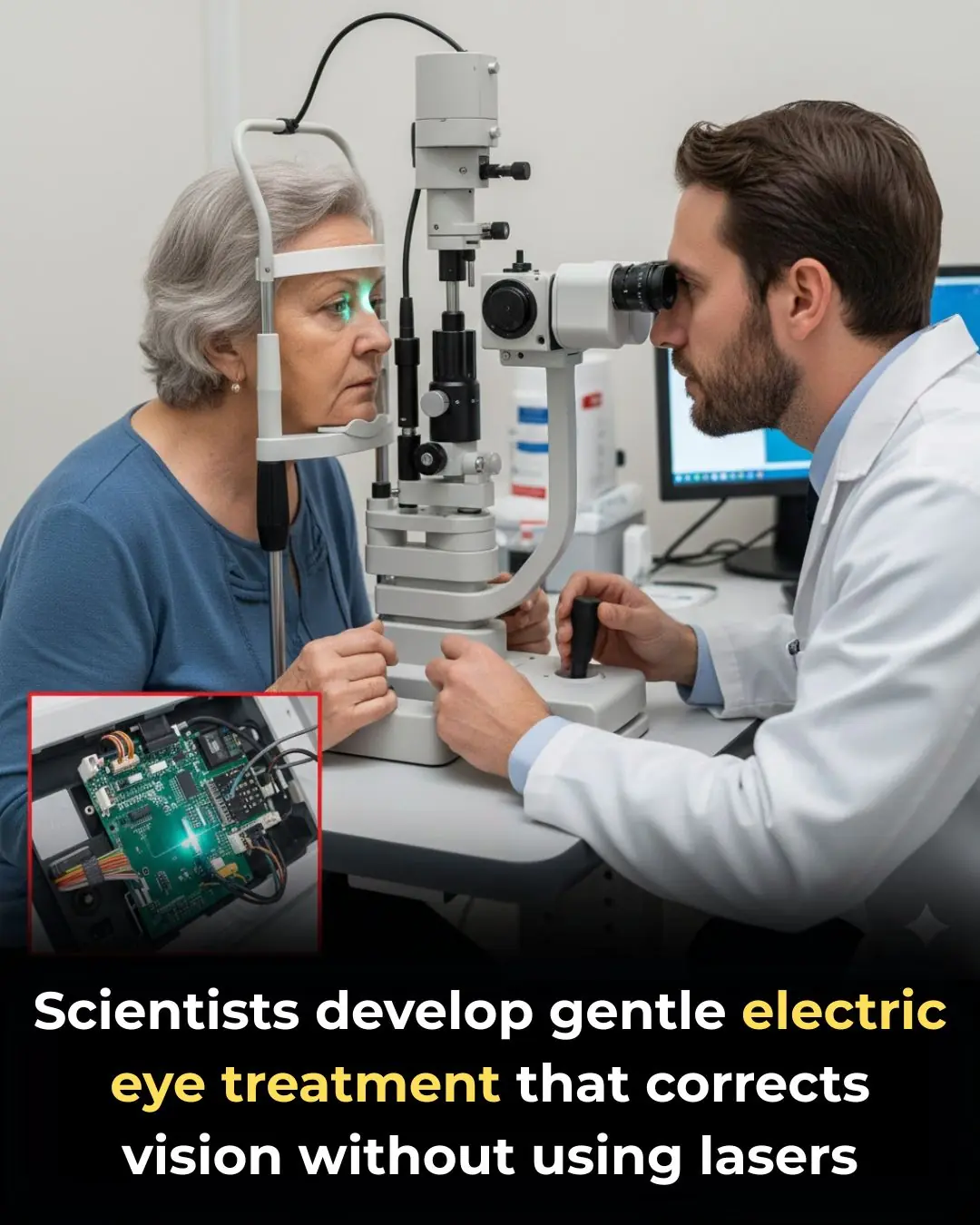
New Vision Correction Technique Reshapes the Cornea Without Surgery
Feeling Relieved Without Your Partner? A Psychologist Says It’s a Warning Sign
