The Brainstem and Pain: New Research, New Understanding
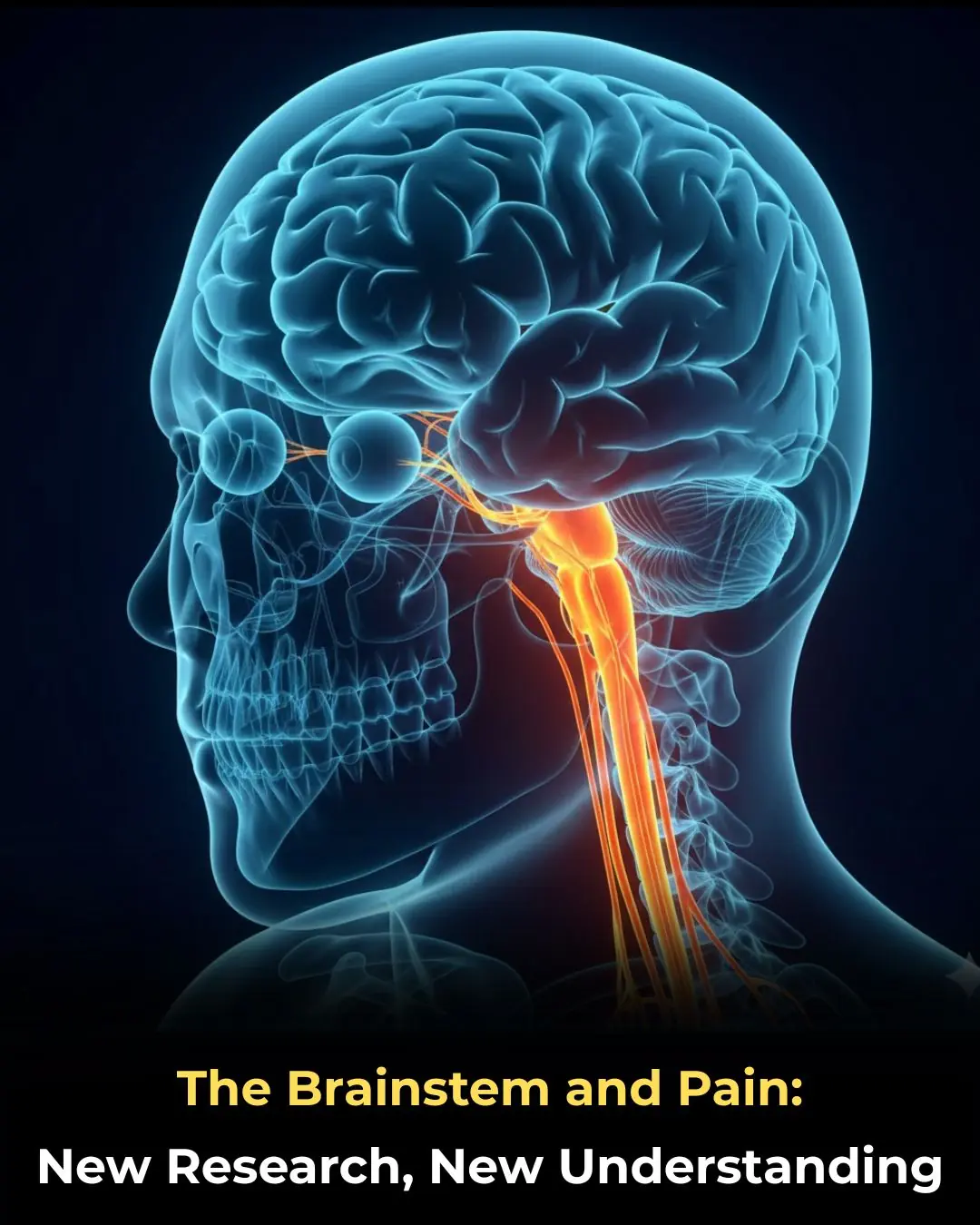
For decades, pain research has focused primarily on the cerebral cortex and spinal cord as the main centers of pain perception. However, emerging scientific evidence is reshaping this view by highlighting the brainstem as a critical regulator of how pain is processed, amplified, or suppressed. These discoveries are transforming our understanding of pain and opening the door to more precise, mechanism-based pain therapies.
What Is the Brainstem and Why Does It Matter?
The brainstem is located at the base of the brain, forming the vital connection between the brain and the spinal cord. It controls essential life-sustaining functions, including:
-
Breathing and heart rate
-
Blood pressure regulation
-
Sleep–wake cycles and consciousness
Beyond these fundamental roles, research now shows that the brainstem plays a central and active role in pain modulation, rather than simply serving as a passive relay station.
New Insights Into How the Brainstem Shapes Pain
1. The Brainstem Actively Modulates Pain Signals
Traditionally, pain signals were thought to travel upward from the body through the spinal cord to higher brain centers. New data demonstrate that the brainstem:
-
Actively adjusts the intensity of pain signals
-
Can enhance or suppress pain before it reaches conscious awareness
This means pain perception is shaped early in the neural pathway, not only in the cortex.
2. Distinct Brainstem Circuits Control Pain Sensitivity
Researchers have identified specialized neural circuits within the brainstem that play opposing roles:
-
Some circuits facilitate pain, increasing sensitivity
-
Others inhibit pain, providing natural analgesia
Disruption or imbalance within these circuits may contribute to:
-
Chronic pain syndromes
-
Widespread pain without clear tissue damage
-
Heightened pain responses to normally mild stimuli
3. Explaining Why Pain Is a Subjective Experience
These findings help explain a long-standing question in medicine:
Why do individuals experience pain so differently, even when the injury is similar?
The answer lies in how each person’s brainstem processes pain signals, influenced by:
-
Psychological stress
-
Anxiety and depression
-
Sleep quality
-
Previous pain experiences
Pain, therefore, is not just a physical sensation but the outcome of a dynamic neurobiological system.
Clinical Implications: Toward More Precise Pain Treatment
1. Mechanism-Based Pain Therapy
Instead of relying solely on broad-spectrum painkillers, future treatments may:
-
Target specific brainstem pathways
-
Restore balance between pain-facilitating and pain-inhibiting circuits
This approach could lead to more effective and personalized pain management.
2. Reducing Dependence on Opioids
A deeper understanding of brainstem pain modulation may:
-
Decrease reliance on opioid medications
-
Lower the risk of addiction and adverse effects
-
Support the development of non-opioid neuromodulation therapies
3. Relevance for Chronic and Unexplained Pain Conditions
These discoveries are especially important for conditions such as:
-
Fibromyalgia
-
Chronic migraine and headache disorders
-
Neuropathic pain
-
Centralized pain syndromes
Targeting brainstem mechanisms may offer new hope for patients who do not respond to conventional treatments.
Conclusion
New research into the brainstem is fundamentally changing how we understand pain. Pain is not merely a direct consequence of tissue injury but the result of complex neural modulation, with the brainstem acting as a key control center. As scientists continue to map these circuits, the future of pain medicine is moving toward precision, personalization, and safer long-term solutions.
News in the same category
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes

Surprising Health Benefits of Purslane (Portulaca oleracea)

Rising Deaths From Stomach Cancer: Doctors Warn — See These 4 Abdominal Signs and Seek Medical Care Immediately

Australia is replacing animal testing with smarter, humane science
Cracked Egg in Your Carton? Here’s When It's Safe to Eat—And When to Toss

Scientists Restore Natural Hearing Using Stem Cells in a Historic Medical Breakthrough
Morning Swelling in Kidney Disease: What Your Body Is Trying to Tell You

Cancer May Show These 2 Warning Signs at Night — Everyone Should Be Aware
Coffee Consumption May Slow Biological Aging in Severe Mental Illness

A French-made artificial heart brings new life to patients once dependent on donor transplants.
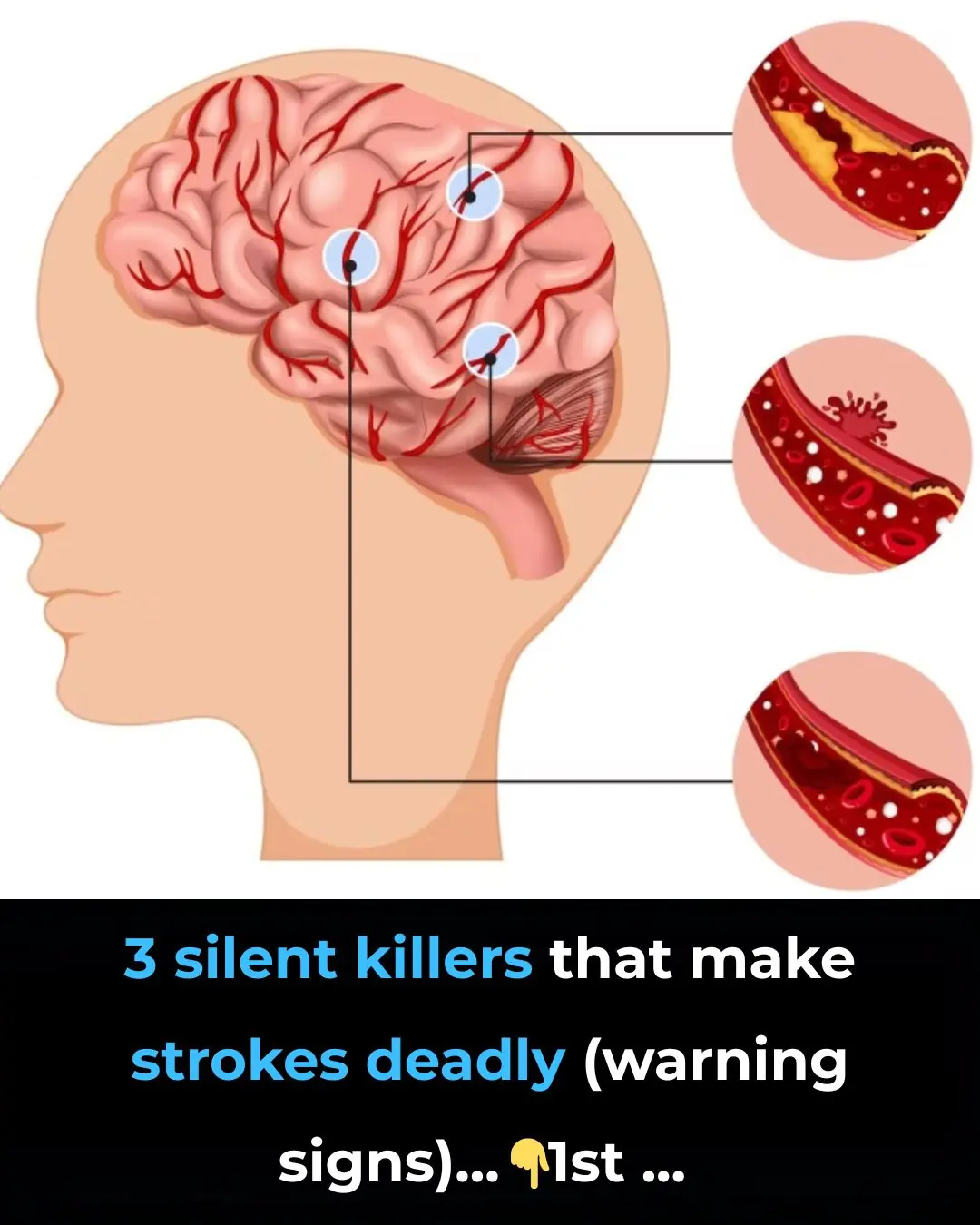
3 silent killers that make strokes deadly (warning signs)

You’d Be Surprised How Your Sleeping Environment Impacts Your Body and Mind

What To Know and Do About Pain Under Your Left Rib Cage
What Causes a Toenail To Turn Black?

7 Foods To Help You Live a Longer, Healthier Life

Why So Many Women Wake Up With Bruises They Don’t Remember Getting
News Post
Advancing Clinical Excellence in IgA Nephropathy

3 types of fruits that are cheap in Vietnamese markets but are considered "pure gold" to protect health

Found this weird skin on my son's ear this morning. Doc appt is a week away. What can I do?

My nana taught me this hack to get rid of dark circles in 5 mins with 0 work. Here’s how it works
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes
Garlic with Olive Oil Over 50: The Irreversible Body Reaction Everyone’s Talking About

Discover How Baking Soda Could Transform Your Skin’s Appearance in Minutes – Even After 70!

What Happens When You Add Just 2 Garlic Cloves a Day to Your Routine – Even After 50!

13 Subtle Signs Your Kidneys May Need Attention

Stop Shaving? Exploring Popular Home Remedies for Hair Removal

Discover the Hidden Power of Ginger Oil: Why Women Over 65 Are Seeing Thicker, Darker Hair Naturally

Top 10 Foods That May Help Reduce Frequent Nighttime Urination (Nocturia)

Why Toothpaste and Baking Soda Aren’t the Answer for Wrinkles and Dark Spots – And What Might Help Instead
James Webb Space Telescope Reveals Hidden Mid-Infrared Flares from the Milky Way’s Central Black Hole
New Vision Correction Technique Reshapes the Cornea Without Surgery
Feeling Relieved Without Your Partner? A Psychologist Says It’s a Warning Sign
