Chinese Scientists Say They Created a Cure for Type 1 Diabetes

A Century-Old Battle Meets a Breakthrough
For more than a century, Type 1 diabetes (T1D) has been like a broken thermostat inside the human body—one that can’t be repaired, only managed. Every day, millions of people around the world rely on insulin injections or pumps to do the job their pancreas no longer can. Managing the condition means a constant balancing act: adjusting meals, activity, stress, and sleep against the invisible—and often unpredictable—swings of blood sugar.
Now, in a quiet laboratory in Beijing, scientists may have uncovered a way to repair the thermostat entirely. Using a patient’s own fat cells, reprogrammed into insulin-producing cells, they have done what generations of doctors and researchers could only dream of: restored the body’s natural ability to make insulin.
The first patient, a 25-year-old woman who had lived with T1D for over a decade, walked away from daily injections and has remained insulin-independent for more than a year.
If this approach proves repeatable, it could rewrite the future of diabetes care. But behind the hopeful headlines lie big questions—about science, safety, access, and whether the world is ready for a true cure.
Understanding Type 1 Diabetes
Unlike Type 2 diabetes, Type 1 is not caused by diet, exercise, or lifestyle choices. Instead, it is an autoimmune condition: the body’s immune system mistakenly attacks and destroys the beta cells in the pancreas, the specialized cells responsible for producing insulin.
Without insulin, glucose cannot enter cells to be used for energy, leading to dangerously high blood sugar (hyperglycemia). The absence of insulin also removes the body’s natural safeguard against blood sugar dropping too low (hypoglycemia), a dangerous state that can lead to confusion, seizures, coma, or even death.
Managing T1D is an around-the-clock task, involving:
-
Continuous blood glucose monitoring with finger-prick tests or advanced sensors.
-
Multiple daily insulin injections or pump adjustments tied to meals, activity, stress, or illness.
-
Constant vigilance to prevent long-term complications like kidney failure, nerve damage, vision loss, and cardiovascular disease.
Even with cutting-edge devices and AI-driven glucose monitors, maintaining stable blood sugar remains a delicate balancing act.
“It’s not just about taking insulin,” says Dr. Daisuke Yabe, a diabetes researcher at Kyoto University. “It’s about replacing the fine-tuned, moment-to-moment control that only a healthy pancreas can provide.”
For decades, the goal of research has gone beyond simply improving insulin delivery—it has been to restore the body’s own insulin production. Until now, all available treatments could only manage the disease, never replace what was lost.
How the New Stem Cell Therapy Works

The experimental treatment developed at Peking University starts with something simple and abundant: fat cells. Far from being mere storage units, fat cells are surprisingly versatile when exposed to the right conditions. Using advanced techniques in regenerative medicine, researchers have developed a five-step process:
-
Extracting the starting material
A small sample of fat tissue is collected through a straightforward outpatient procedure, providing an ample supply of cells to work with. -
Rewinding the cells to a “pluripotent” state
Through a refined chemical process led by researcher Dr. Deng Hongkui, these cells are converted into induced pluripotent stem cells (iPSCs)—cells that, like embryonic stem cells, have the potential to become virtually any cell type in the body. -
Guiding the transformation
The iPSCs are coaxed into becoming insulin-producing islet cells, closely mimicking the beta cells of the pancreas. These lab-grown cells must not only produce insulin but also respond dynamically to changes in blood glucose levels. -
Transplanting to a novel location
Unlike older methods that implanted islets in the liver, this technique places them in the abdominal muscle, where they can be easily monitored through imaging and, if necessary, removed—reducing the risk of complications. -
Restoring natural insulin control
Once transplanted, the new cells integrate into the surrounding tissue and begin releasing insulin in response to blood sugar levels. In the first patient, this restored enough insulin production to eliminate external injections within 75 days. Her blood sugar levels have remained within a healthy range over 98% of the time for more than a year.
This approach stands apart from earlier experimental therapies, which often relied on donor cells or unrelated stem cells—solutions that required lifelong immunosuppressants to prevent rejection. Using a patient’s own cells dramatically lowers this risk.
Challenges, Unknowns, and Scientific Caution

While this breakthrough is remarkable, experts emphasize that a single success does not equal a universal cure.
1. Long-term durability
It’s still unclear how long the reprogrammed cells will remain functional. Transplanted cells can weaken over time, losing their ability to sense and respond to blood sugar.
2. Autoimmune risk
Because T1D is an autoimmune condition, the body’s immune system could attack the new beta cells even though they originate from the patient. The first patient avoided this problem due to immunosuppressants taken for a previous liver transplant, but most patients won’t have that protection. Researchers are investigating ways to shield the new cells from immune attack.
3. Scalability and cost
Reprogramming fat cells into functional beta cells is labor-intensive and expensive, requiring highly specialized equipment and expertise. Scaling this therapy to treat millions globally would demand significant infrastructure and regulatory approvals.
4. Limited data
So far, only three patients have undergone the procedure, with published results available for just one. Larger clinical trials are needed to confirm safety and effectiveness.
5. Timelines and reality checks
Even in a best-case scenario, it could take years—if not a decade—before this therapy becomes widely available. For now, insulin remains the gold-standard treatment.
Global Implications and Industry Challenges

If proven safe, effective, and scalable, this therapy could transform global health. Type 1 diabetes affects roughly nine million people worldwide, while Type 2 diabetes impacts over 400 million. For both, insulin is a lifelong lifeline, accompanied by constant monitoring and risk of complications.
A shift in healthcare
For individuals, a functional cure could mean freedom from needles, pumps, and relentless monitoring. For healthcare systems, it could significantly reduce costs and long-term complications, saving billions annually.
Economic ripple effects
The global insulin market—worth over $20 billion annually in the U.S. alone—could face disruption. History shows that when groundbreaking treatments threaten entrenched markets, industry pushback, regulatory delays, or limited promotion often follow.
Geopolitical dynamics
That this breakthrough originates from China adds a geopolitical dimension. Traditionally, Western institutions have led in biotech innovation, but this success could shift influence and spark international competition or collaboration.
Equity and access
Even if the therapy succeeds, not everyone will have equal access. Wealthier nations may adopt it first, while low- and middle-income regions—where diabetes rates are climbing—could face years or decades of delay. Advocacy for affordable and equitable access will be critical.
What It Means for Patients Now

For people living with T1D, hearing that someone is living insulin-free is both thrilling and bittersweet. The therapy is still in its infancy, tested in only a handful of people, and widespread availability remains years away.
For now:
-
Insulin remains essential.
-
Advanced technologies like continuous glucose monitors and automated insulin pumps are improving quality of life and reducing risk.
-
Advocacy and patient engagement are vital to ensuring breakthroughs are tested rigorously and made accessible globally.
A Future Within Reach
The story of a young woman in Beijing, now free from insulin after years of dependence, is a beacon of possibility. It shows that the dream of restoring natural insulin production is no longer science fiction.
But the path forward will require persistence—years of clinical testing, cross-border collaboration, and a commitment to equitable access. Whether this therapy transforms from a medical milestone into a universal cure will depend on the combined efforts of researchers, regulators, advocates, and the global diabetes community.
For now, the message is clear: keep managing today’s reality while preparing for tomorrow’s breakthroughs. What was once impossible is now within reach—and that, in itself, is a remarkable shift.
News in the same category
Researchers Find Higher Intelligence Is Correlated With Left-Wing Beliefs and Seems to Be Genetic

Urgent Health Warning Issued After Pigs With ‘Neon Blue’ Flesh Are Discovered in One Specific Part of the Us

'Hostile' comet aimed at Earth could obliterate the world's economy 'overnight' if it hits
Iconic movie sequel delayed until 2027 after online sleuths 'guessed the plot'

Don’t Sleep With Your Pets
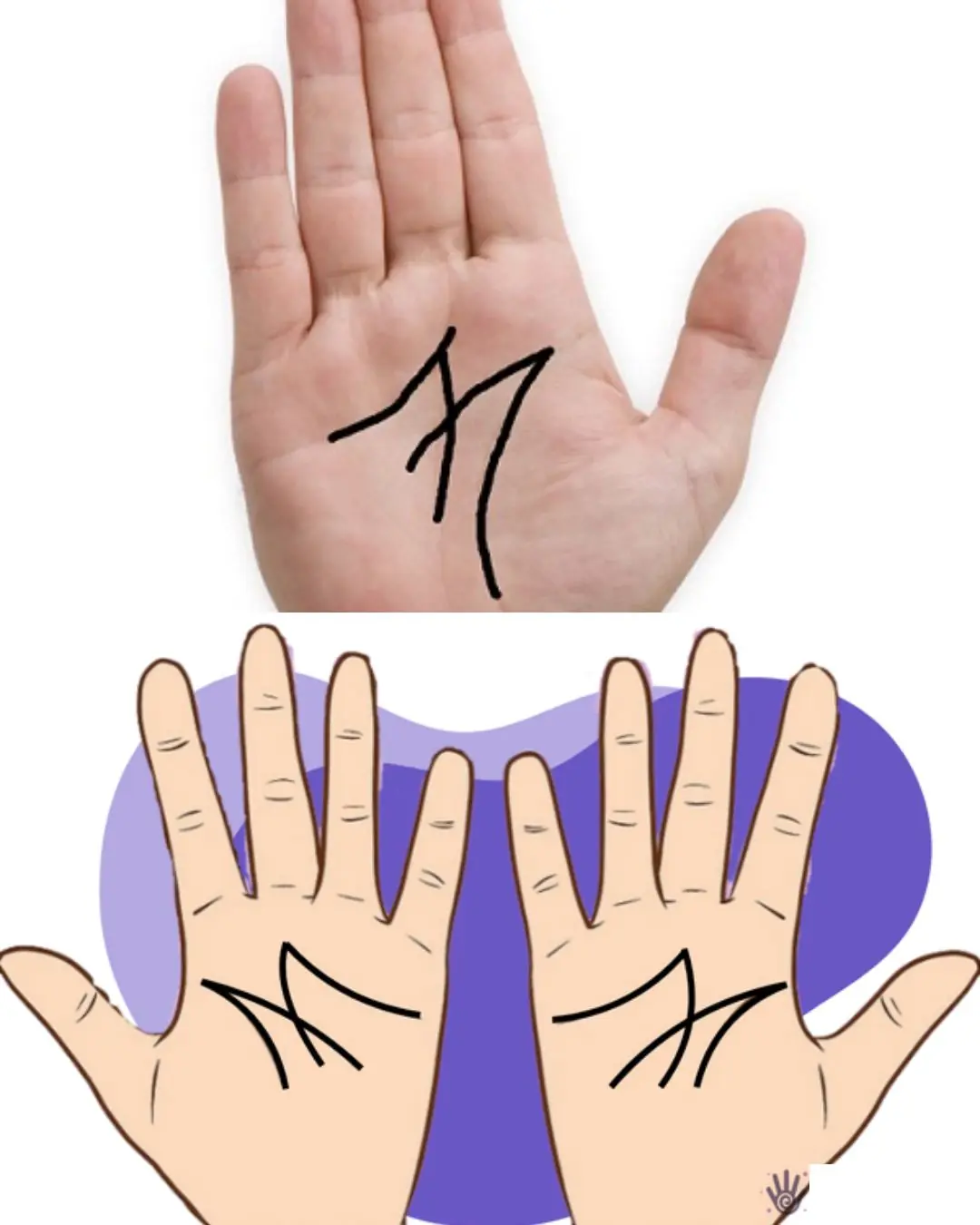
The Secret Meaning of the Letter “M” on Your Palm
The Remarkable Journey of Tru Beare, Who Was Born Weighing Only One Pound

Researchers Create Injectable Hydrogel to Boost Bone Strength

If You Have Moles on This Part of Your Body
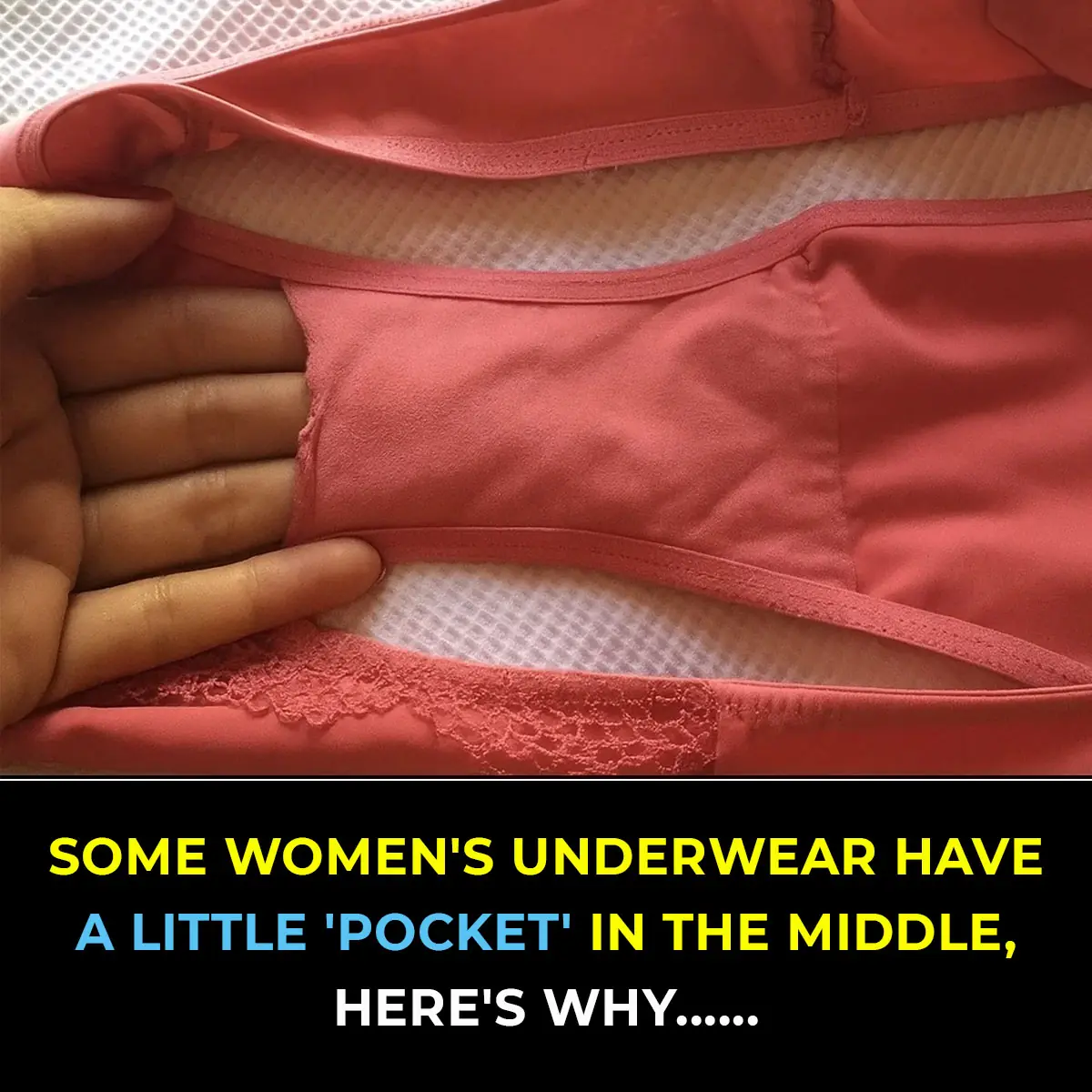
The Purpose of the Small Pocket in Women’s Underwear
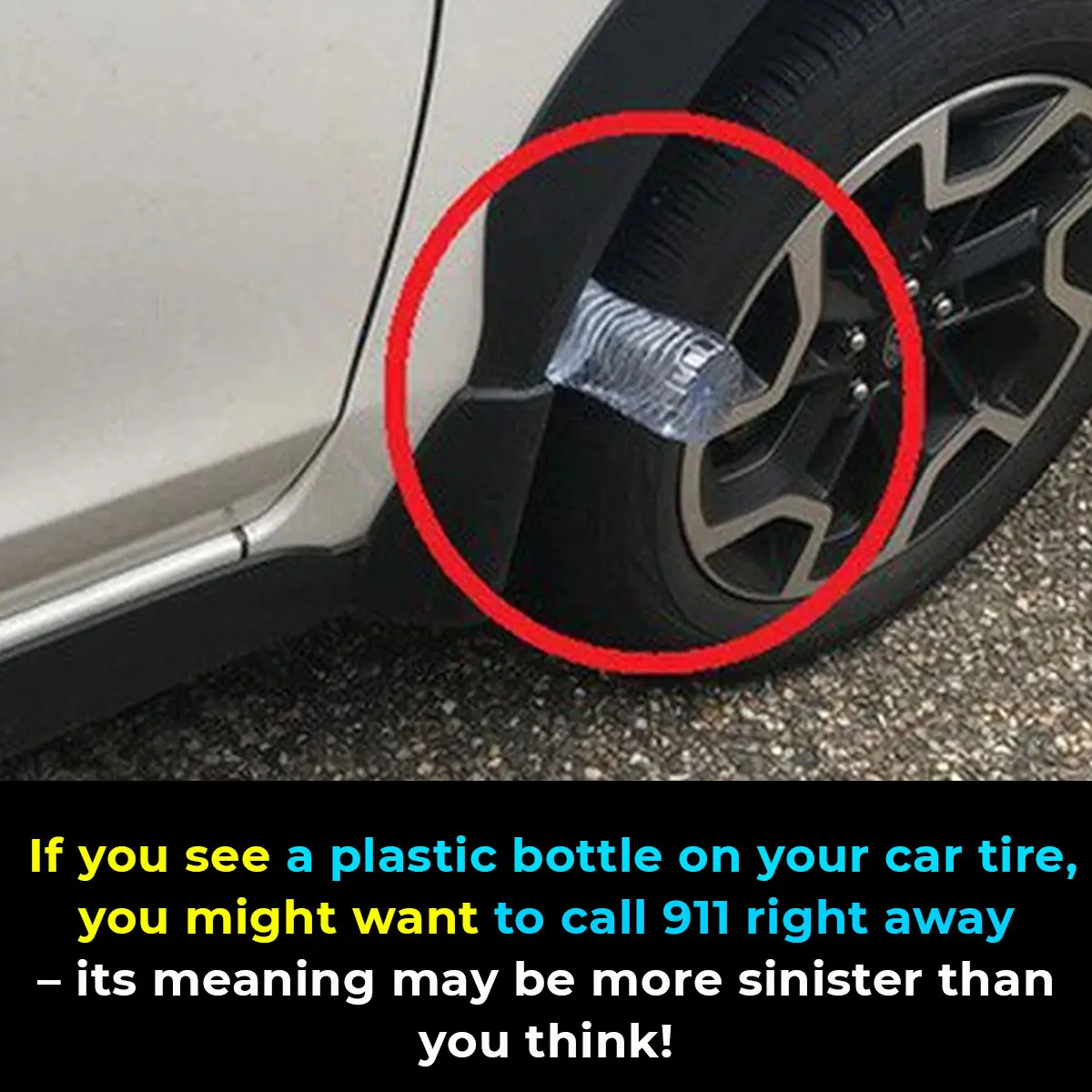
Beware of the Plastic Bottle Scam: A New Car Theft Tactic

Rob Gronkowski forgot he invested $69,000 in Apple and ten years later the value has completely changed his net-worth

Scientists discover that powerful side effect of Ozempic could actually reverse aging

Scientists warn ancient Easter Island statues could vanish in a matter of years
NASA astronaut describes exactly what space smells like and it's not what you'd expect

Subtle Signs Your Passed Loved One Is Watching Over You
What Does a Thumb Ring Really Mean
News Post

Parasite Cleanses: Do They Really Improve Your Gut Health — and Are They Safe?

8 Teas to Drink for a Healthier Body and Mind

The Hidden Truth About Tinnitus: Why That Ringing in Your Ears Shouldn’t Be Ignored
Over time, repeated noise trauma damages tiny hair cells inside the cochlea, which cannot regenerate, resulting in permanent hearing changes and tinnitus.

DIY Turmeric & Ginger Shots to Fight Inflammation, Boost Immunity & Soothe Your Gut

Coconut water: Is It Good for You, Nutrition, Benefits, Side Effects (Science Based)

Clean Arteries: 10 Foods to Eat Daily

10 Warning Signs of Parasites in Your Body
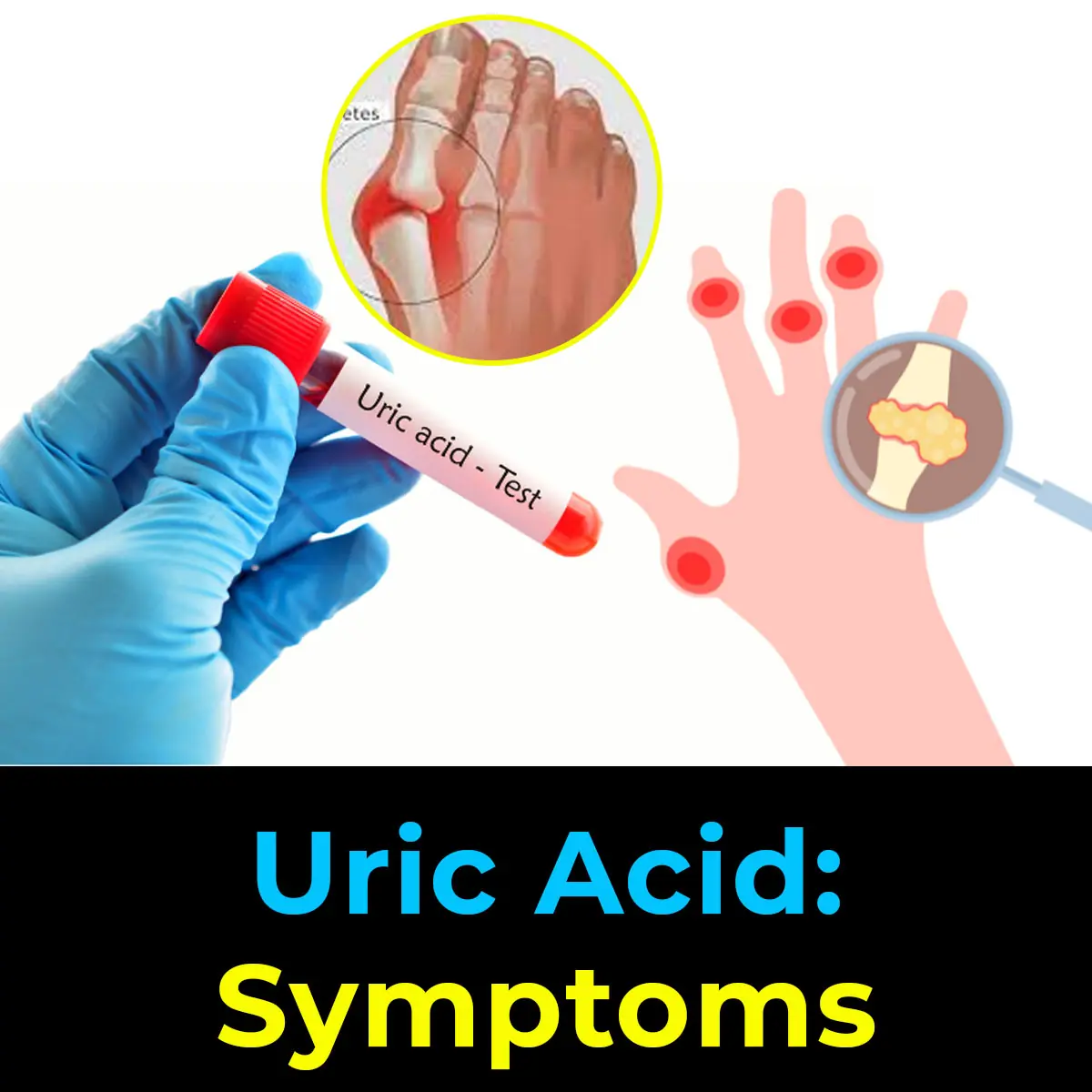
Diet and Uric Acid: Foods to Avoid for Gout Prevention

Hiker Encounters Massive Snake Camouflaged Along South Carolina Creek

8 Foods That Help Eliminate Cancer Cells

David Quammen, the COVID Predictor Warns of New Pandemic Threats
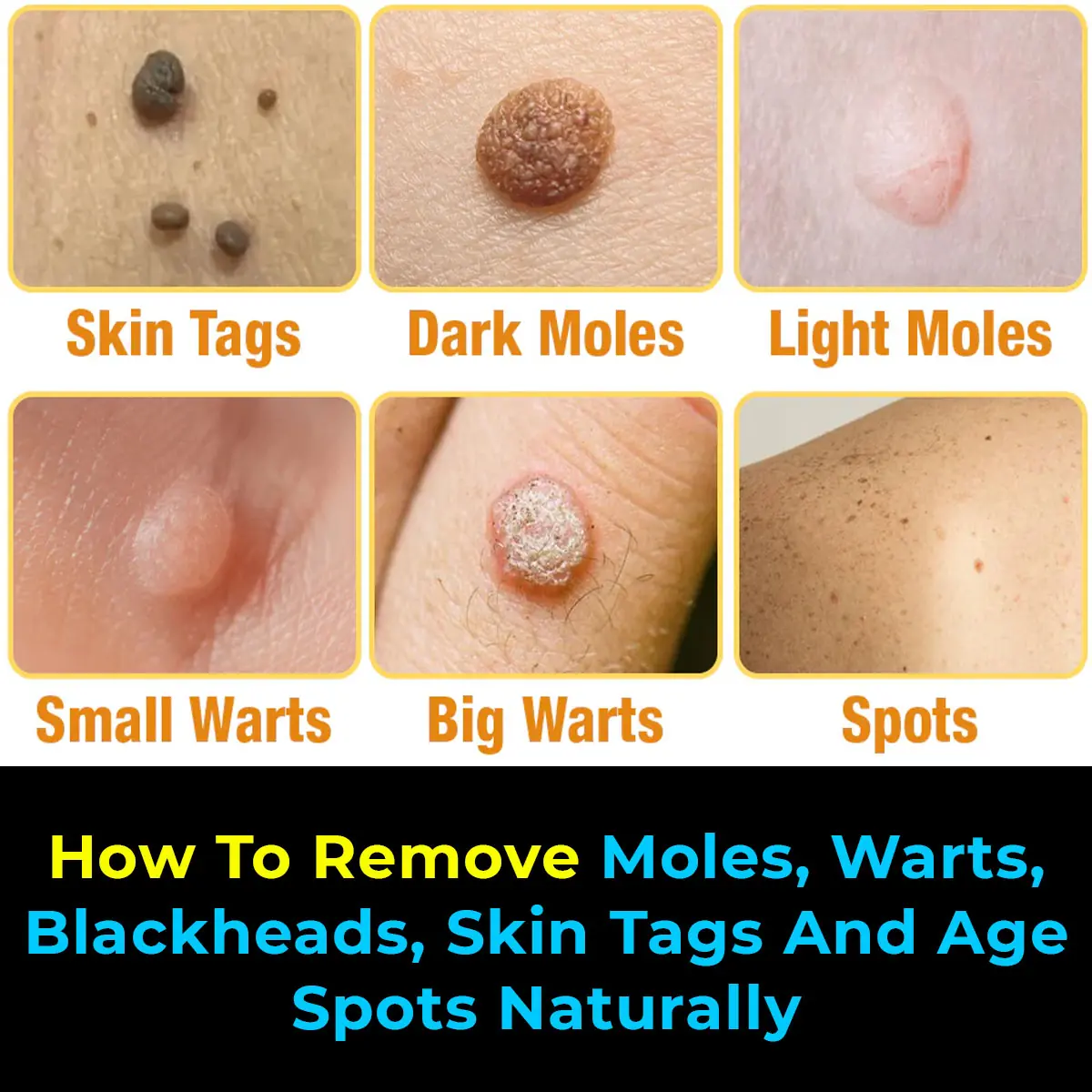
Natural Remedies to Address Skin Tags, Warts, and Blackheads
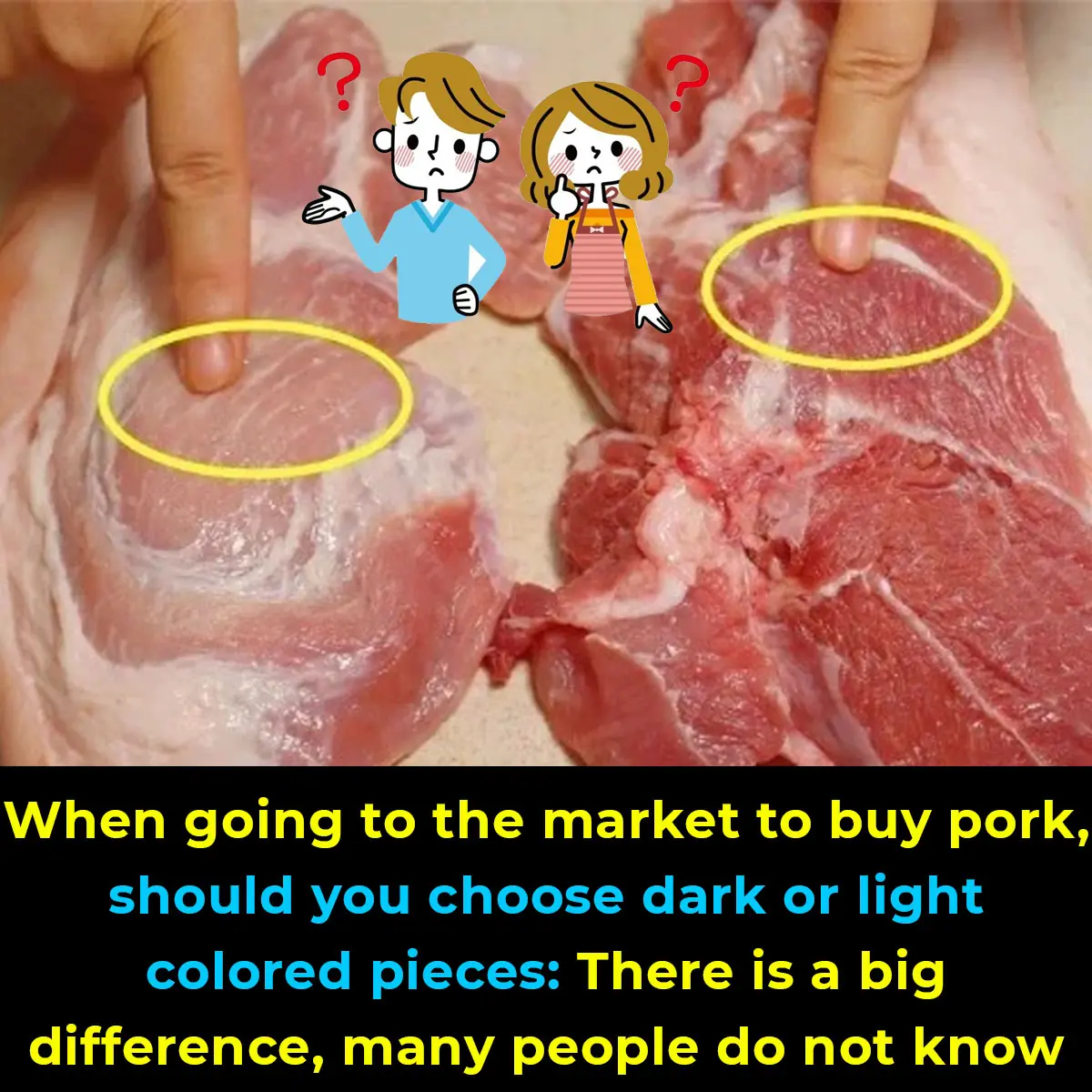
Tips for Selecting Fresh Pork at the Market
The Deficiency of These Vitamins Contributes to Panic Attacks
Researchers Find Higher Intelligence Is Correlated With Left-Wing Beliefs and Seems to Be Genetic

Urgent Health Warning Issued After Pigs With ‘Neon Blue’ Flesh Are Discovered in One Specific Part of the Us

25-Year-Old Groom Dies from Acute Liver Failure After Eating Chicken – Doctors Warn of One Critical Danger!
Doctors caution people with pre-existing liver conditions, weakened immune systems, or chronic illnesses to exercise extra care when handling poultry and other high-risk.
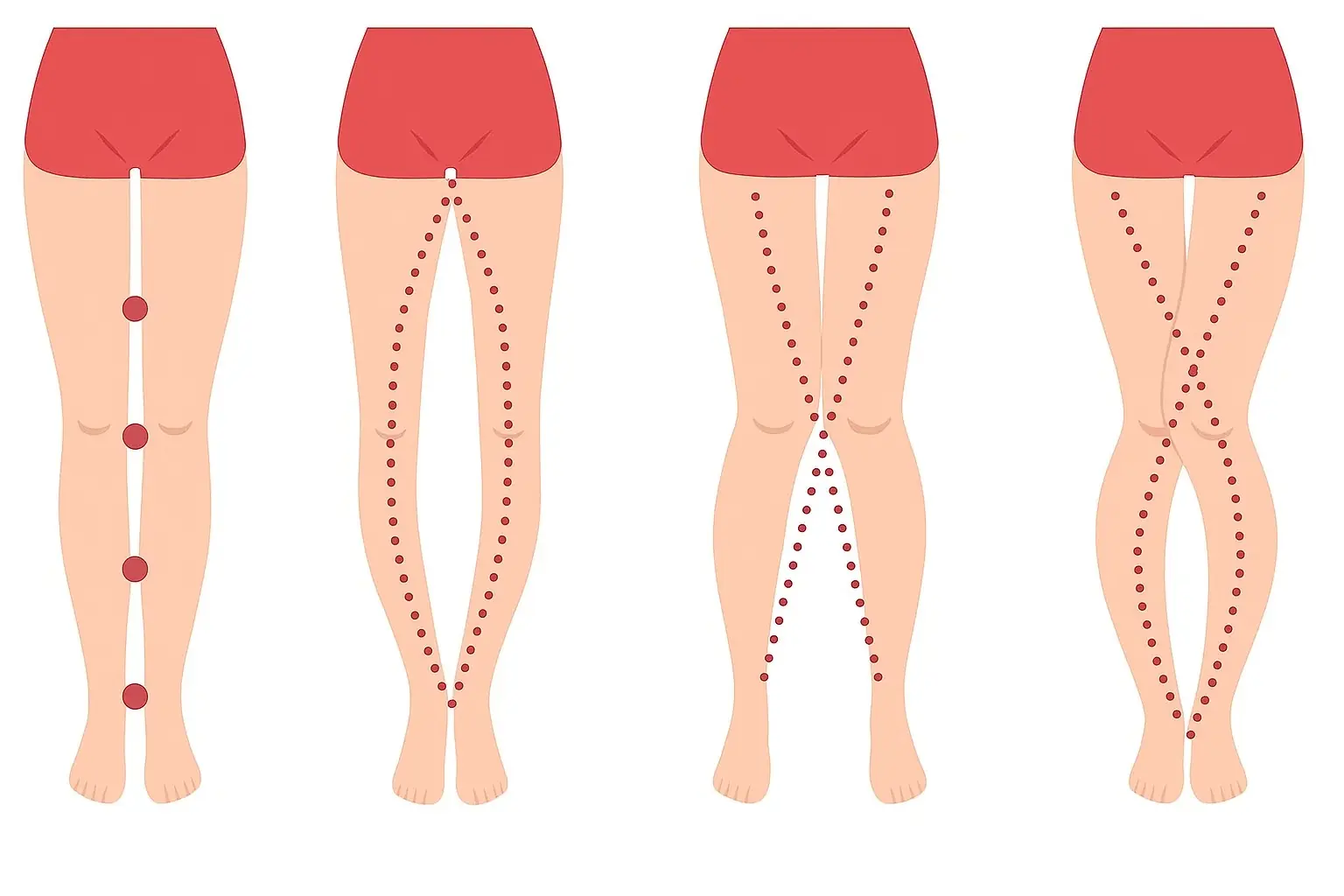
What Your Legs Can’t Say, Your Vagina Can — The Truth About the Female Body Most People Don’t Know
9 Areas Where Itching Could Signal Malignant Tumors — #7 Happens Most Often

The World’s Deadliest Food Kills 200 People Every Year — Yet 500 Million Still Eat It
Despite its deadly reputation, millions of people continue to eat this every day without issue.