Tapering Antidepressants: What Strategy Works Best?

For millions of people worldwide, antidepressants are a cornerstone of treatment for major depressive disorder. Yet once symptoms remit and patients begin to consider stopping medication, clinicians and patients alike face a critical question: How can antidepressants be discontinued safely without increasing the risk of relapse?
A growing body of evidence now provides clearer guidance. According to a new comprehensive analysis, adults with remitted depression can reduce or discontinue antidepressants without significantly increasing relapse risk—provided the process is slow, structured, and supported by psychological care. In contrast, abrupt or rapid discontinuation markedly increases the likelihood of depressive relapse.
These findings reinforce a shift toward evidence-based deprescribing and challenge outdated practices that underestimate the complexity of antidepressant withdrawal.
The Challenge of Discontinuing Antidepressants
Antidepressant use has increased steadily over the past two decades, with many patients remaining on medication for years—even after achieving symptom remission. While long-term treatment is appropriate for some individuals, others may wish to reduce or stop medication due to side effects, life changes, pregnancy planning, or personal preference.
Historically, discontinuation has often been approached inconsistently, with wide variation in tapering schedules and limited guidance on best practices. This has led to confusion between withdrawal symptoms and true depressive relapse, sometimes resulting in unnecessary long-term medication use.
What the New Evidence Shows
The new analysis pooled data from multiple randomized and observational studies involving adults whose depression was in remission. Researchers compared outcomes among patients who:
-
Continued antidepressants at a full therapeutic dose
-
Gradually tapered medication with structured psychological support
-
Discontinued antidepressants abruptly or rapidly
The results were striking:
-
Slow tapering combined with psychological support resulted in relapse rates similar to those seen in patients who remained on full-dose antidepressants.
-
Abrupt or rapid discontinuation significantly increased the risk of relapse.
-
Withdrawal symptoms were frequently mistaken for depressive recurrence when tapering was too fast.
These findings suggest that relapse is not an inevitable consequence of stopping antidepressants—but rather a preventable outcome when discontinuation is poorly managed.
Why Slow Tapering Matters
Antidepressants induce long-term neurobiological adaptations, including changes in serotonin signaling, receptor sensitivity, and neural plasticity. When medication is stopped suddenly, the brain may struggle to rebalance these systems, leading to withdrawal symptoms such as:
-
Anxiety and agitation
-
Insomnia
-
Dizziness or “brain zaps”
-
Mood instability
These symptoms can closely resemble depressive relapse, making clinical assessment challenging.
Gradual tapering allows the brain time to adjust incrementally, reducing physiological stress and minimizing withdrawal-related symptoms that might otherwise undermine recovery.
The Role of Psychological Support
One of the most important insights from the analysis is the protective effect of psychological support during tapering. Patients who received structured interventions—such as cognitive behavioral therapy (CBT), mindfulness-based cognitive therapy (MBCT), or regular clinical monitoring—had significantly better outcomes.
Psychological support helps patients:
-
Differentiate withdrawal symptoms from relapse
-
Develop coping strategies for stress and emotional fluctuations
-
Maintain confidence during the tapering process
-
Address residual cognitive or behavioral patterns linked to depression
This reinforces the idea that antidepressants should not be viewed as standalone solutions but as part of a broader, integrated treatment plan.
Implications for Clinical Practice
The findings strongly support updated clinical guidelines that emphasize careful, individualized deprescribing rather than abrupt cessation. Experts increasingly recommend that clinicians:
-
Assess relapse risk based on patient history, number of prior episodes, and psychosocial context
-
Develop a personalized tapering schedule that may span weeks or months
-
Provide or refer for psychological support during and after tapering
-
Educate patients about expected withdrawal symptoms and warning signs of relapse
Importantly, deprescribing should be framed as a collaborative process, not a one-size-fits-all directive.
Reducing Stigma and Empowering Patients
For many patients, difficulty stopping antidepressants has been interpreted as evidence of “dependency” or personal weakness. The new evidence challenges this narrative by highlighting the biological basis of withdrawal symptoms and the importance of proper tapering.
Understanding that relapse risk can be minimized with the right strategy may empower patients to make informed decisions about their treatment—without fear or guilt.
What This Means for the Future of Depression Care
As mental health care evolves, the focus is shifting from simply initiating treatment to managing the entire course of illness—including recovery and medication discontinuation. This research underscores the need for:
-
Better clinician education on deprescribing strategies
-
Clearer patient-facing guidance on tapering expectations
-
Expanded access to psychological therapies during medication transitions
By aligning clinical practice with emerging evidence, healthcare systems can support safer, more patient-centered approaches to antidepressant use.
Conclusion
Adults with remitted depression do not necessarily need to remain on lifelong antidepressant therapy to prevent relapse. When antidepressants are tapered slowly and accompanied by psychological support, patients can achieve outcomes comparable to continued full-dose treatment.
In contrast, abrupt or rapid discontinuation significantly increases relapse risk—highlighting the importance of careful, evidence-based deprescribing.
As guidelines continue to evolve, these findings offer reassurance that stopping antidepressants can be done safely—not by rushing the process, but by respecting the brain’s need for time, support, and thoughtful care.
News in the same category

The Brainstem and Pain: New Research, New Understanding
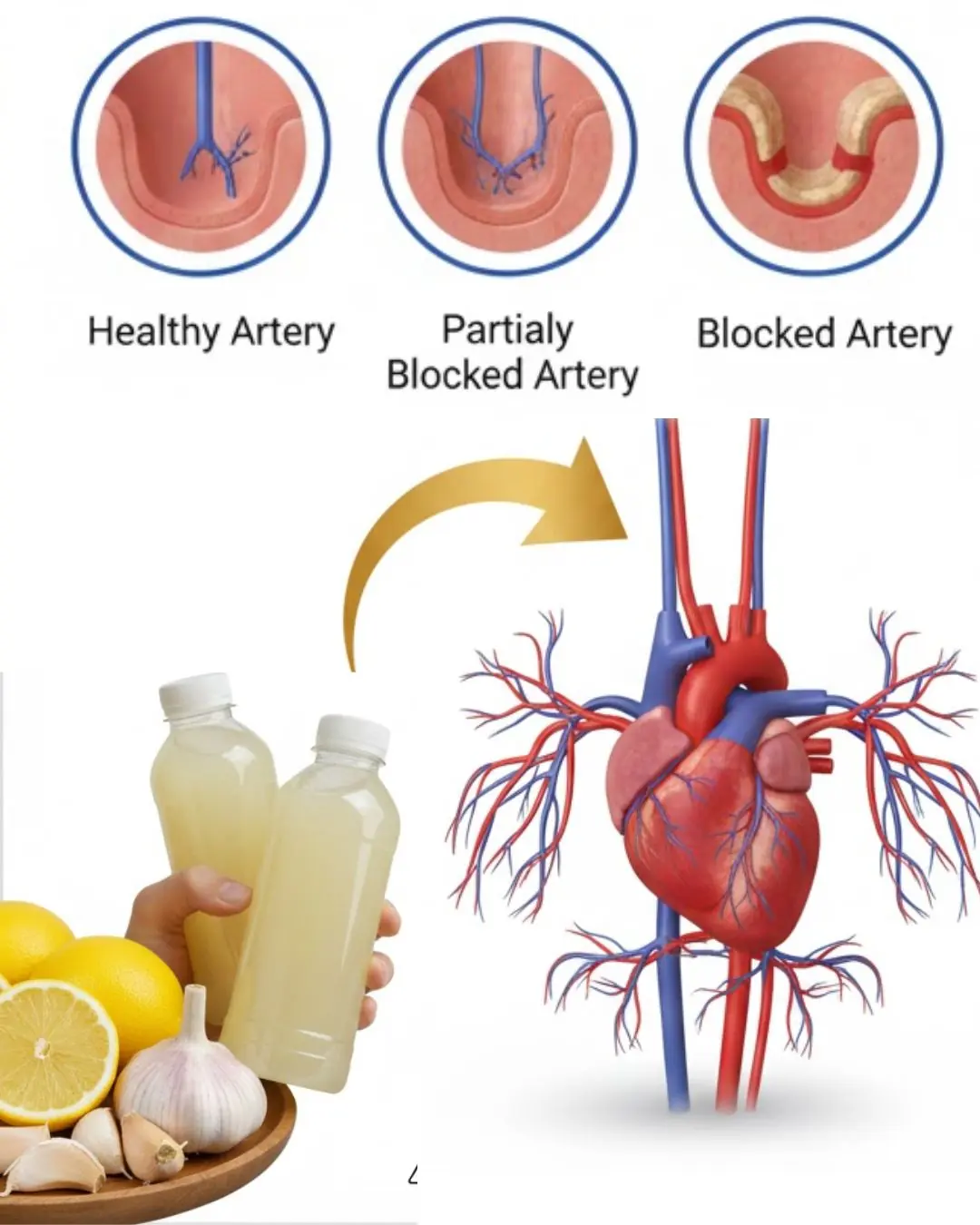
Could a Simple Bedtime Drink with Three Common Ingredients Support Your Heart Health?
Between Supplement Hype and Evidence: A Clinical Guide for Informed Use
Current Cardiac Screening Tools Miss Nearly Half of First Heart Attacks, Study Finds

Could Bone Broth Support Healthy Knee Cartilage as You Age?

Top 7 Best Drinks Diabetics Can Enjoy at Night to Support Healthy Blood Sugar Levels!

Papaya Leaves for Hair: A Natural Way to Support Healthier, Shinier Strands
Protect Your Eyes Naturally: 3 Powerful Seeds and 1 Fruit Every Senior Should Know About

Power Naps: The Benefits, How Long They Should Be, and When They Work Best
5 Early Signs and Symptoms of Ulcerative Colitis

8 Potential Health Benefits of Kombucha

Diagnosed with End-Stage Stomach Cancer, I Painfully Realized: 3 Foods Left Too Long in the Refrigerator Can Become “Accomplices” to Cancer

5 Detox Baths to Remove Aches, Pains and Toxins + Fragrant Bath Melts Recipe
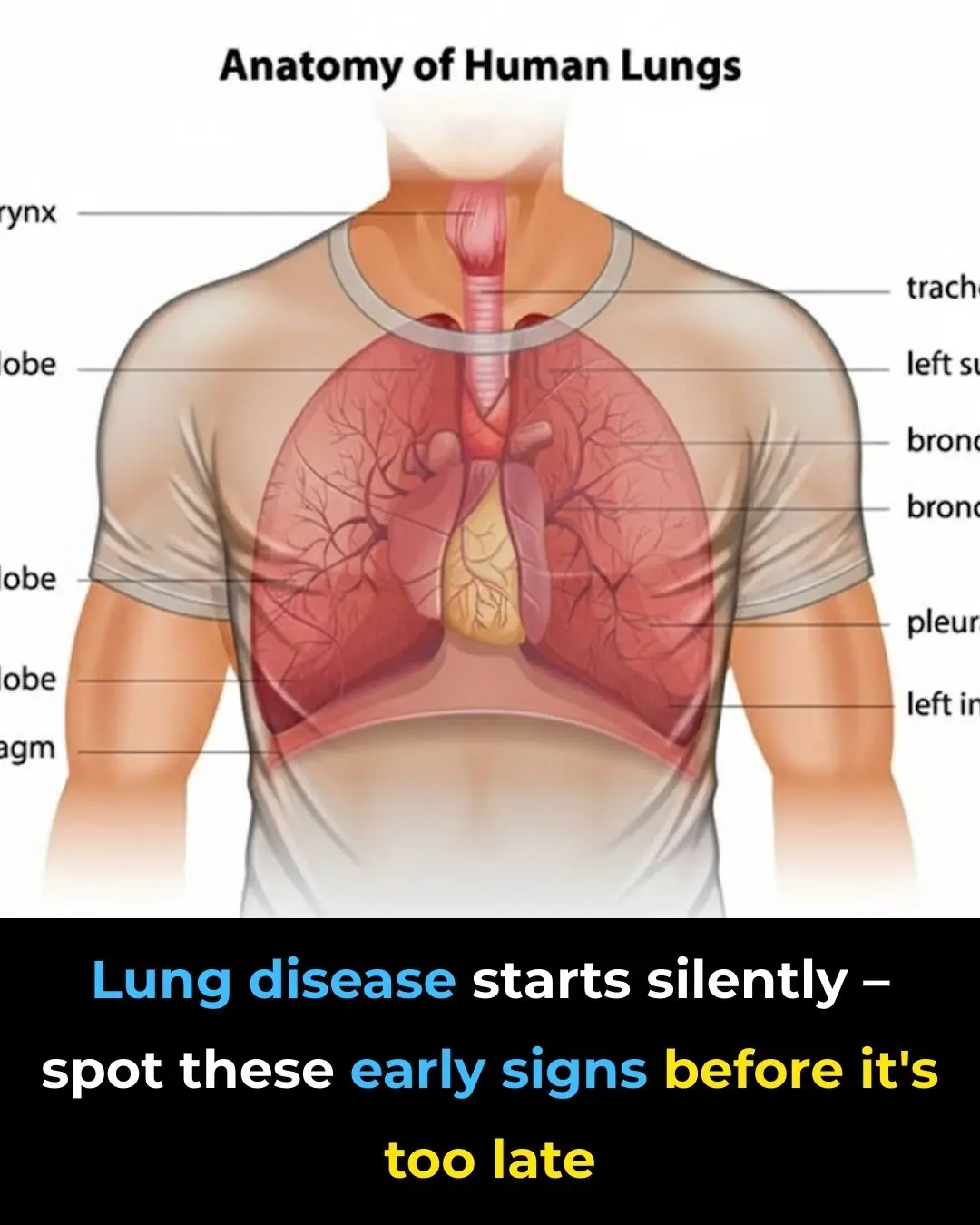
Early Signs of Lung Disease & How to Strengthen Your Lungs

5 things you absolutely SHOULDN'T do in the morning if you don't want your cancer cells to "grow like wildfire"

Emerging Flu Variant ‘Subclade K’ Raises Global Health Concerns Across the US, UK, and Beyond
A New Alternative to Reading Glasses: Eye Drops for Age-Related Near-Vision Loss
News Post

Bananas, Garlic, and Dates: The Powerful Health Combo
A Complete Guide to Breast Cancer Prevention

What Can Happen When Women Lack Sexual Intimacy?
After 30 years of my life, I learned that microwave ovens have this function
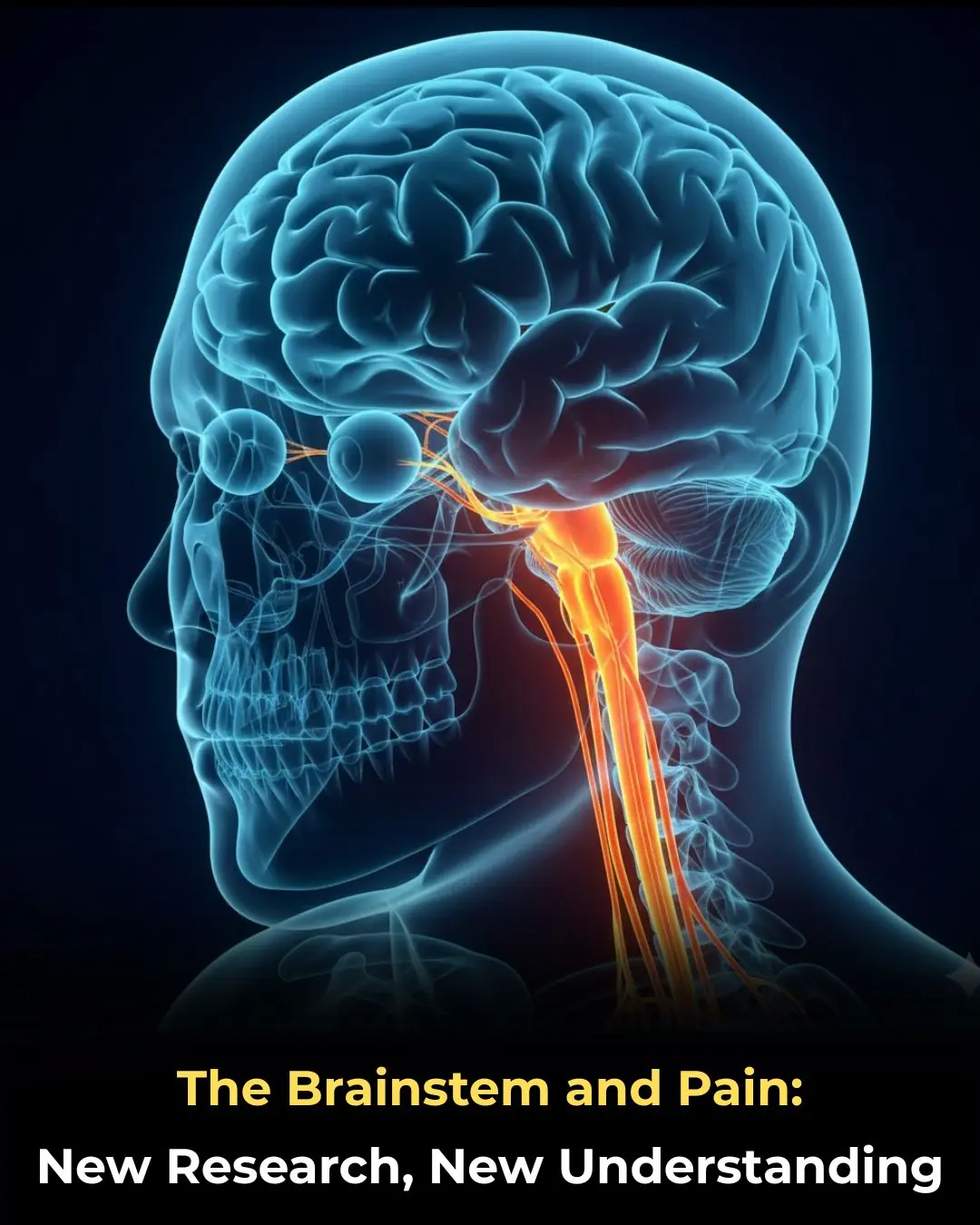
The Brainstem and Pain: New Research, New Understanding
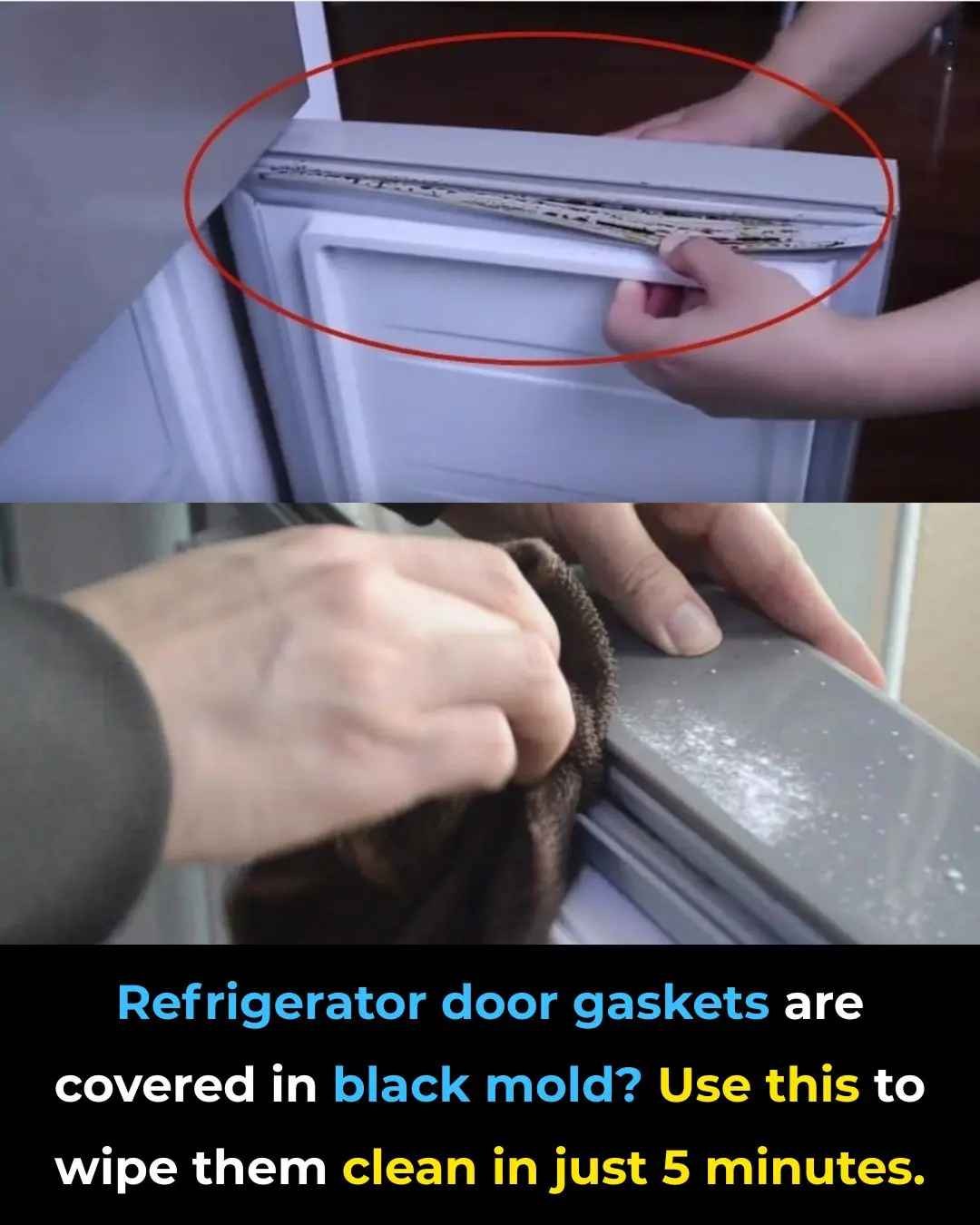
Black Mold on Refrigerator Door Seals? Use This Simple Trick to Clean It in Just 5 Minutes

Five Extremely Dangerous Types of Meat You Should Avoid
10 Probiotic Foods to Improve Your Gut Health Naturally
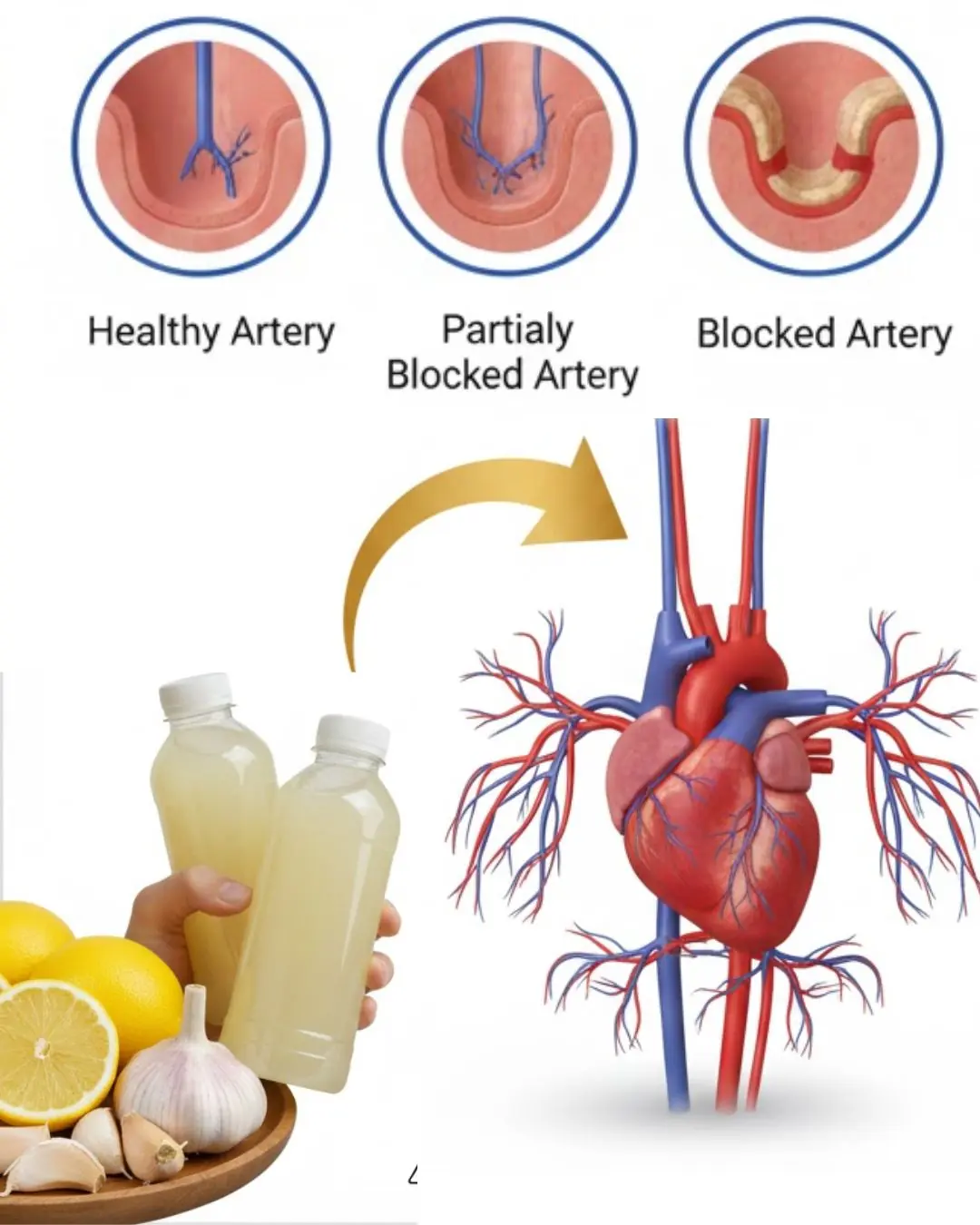
Could a Simple Bedtime Drink with Three Common Ingredients Support Your Heart Health?
What kind of fruit is so familiar that most people eat it when it's ripe but don't know that the green fruit is considered the "architect" of the intestines?

A TV Viewer’s Sharp Eye Helped Save Flip or Flop Star Tarek El Moussa’s Life
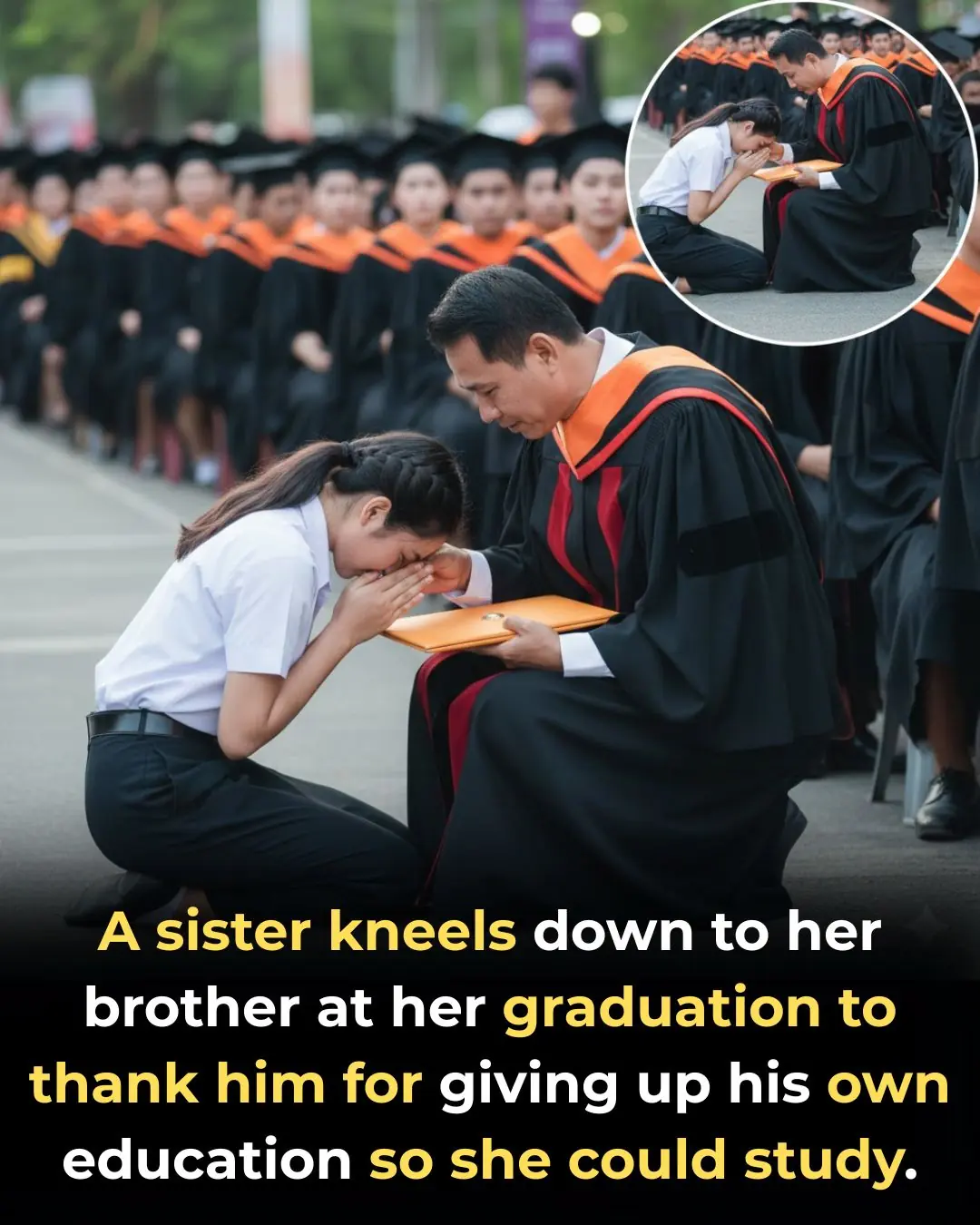
Graduate Kneels to Thank Brother Who Gave Up School for Her

32 Years of Service: Community Saves Elderly Carabao in the Philippines From Slaughter

A Father at Work, a Baby’s Smile, and a Moment That Touched Millions
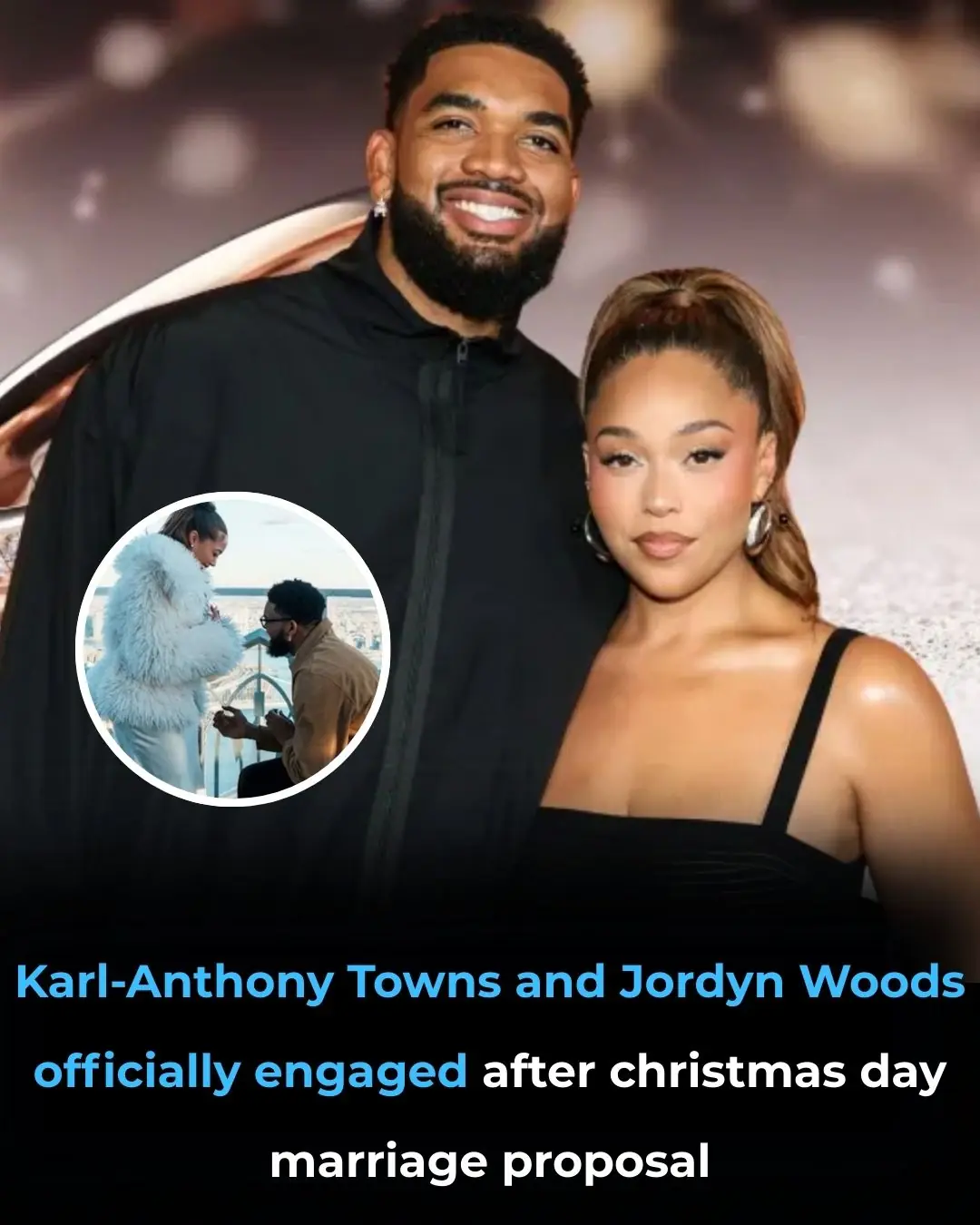
Jordyn Woods is engaged to Karl-Anthony Towns — see the massive engagement ring set to spark trends in 2026
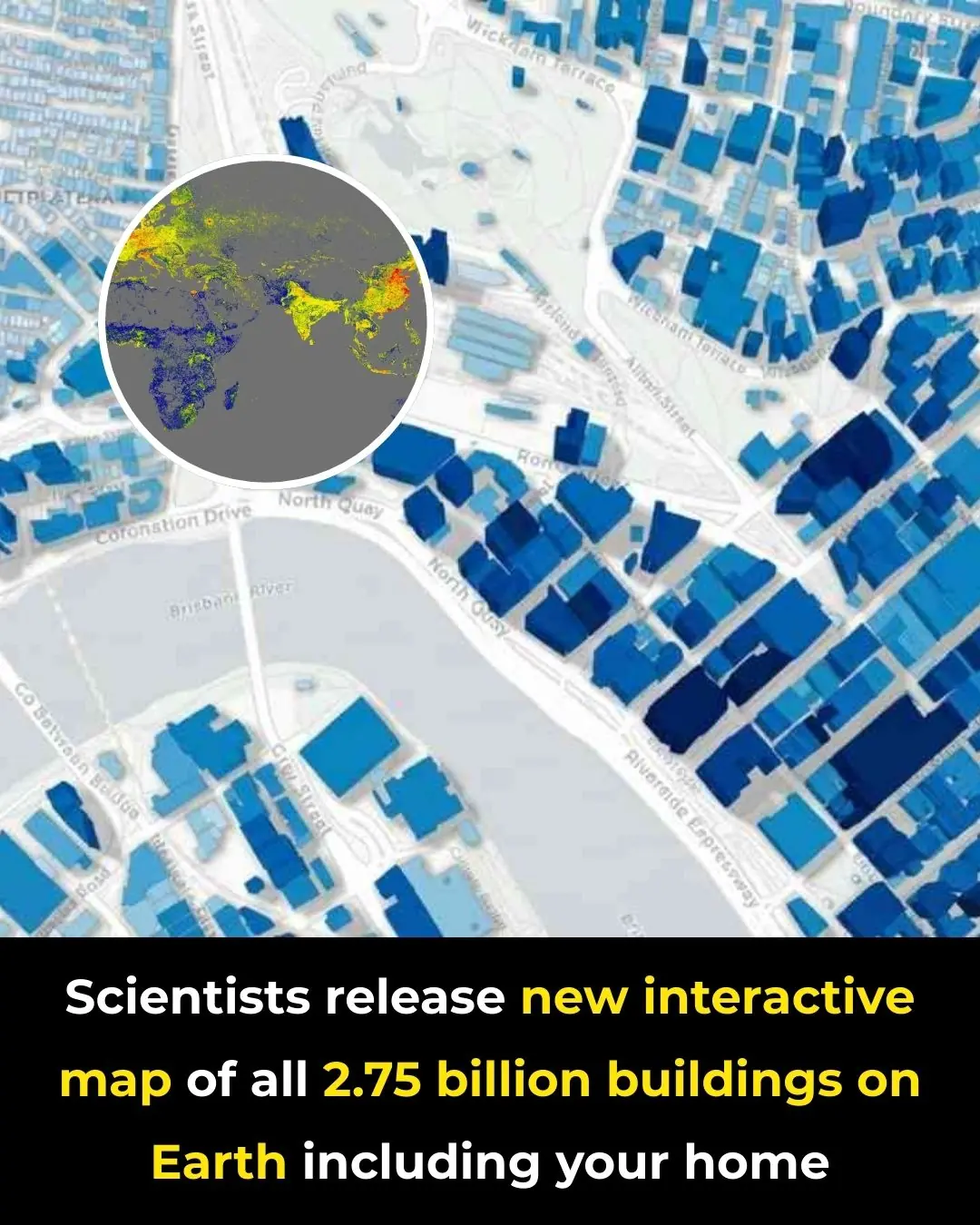
A New Global Atlas Maps Every Building on the Planet in Unprecedented Detail

A Bed on Wheels: A Chinese Inventor’s Unusual Take on Personal Transportation
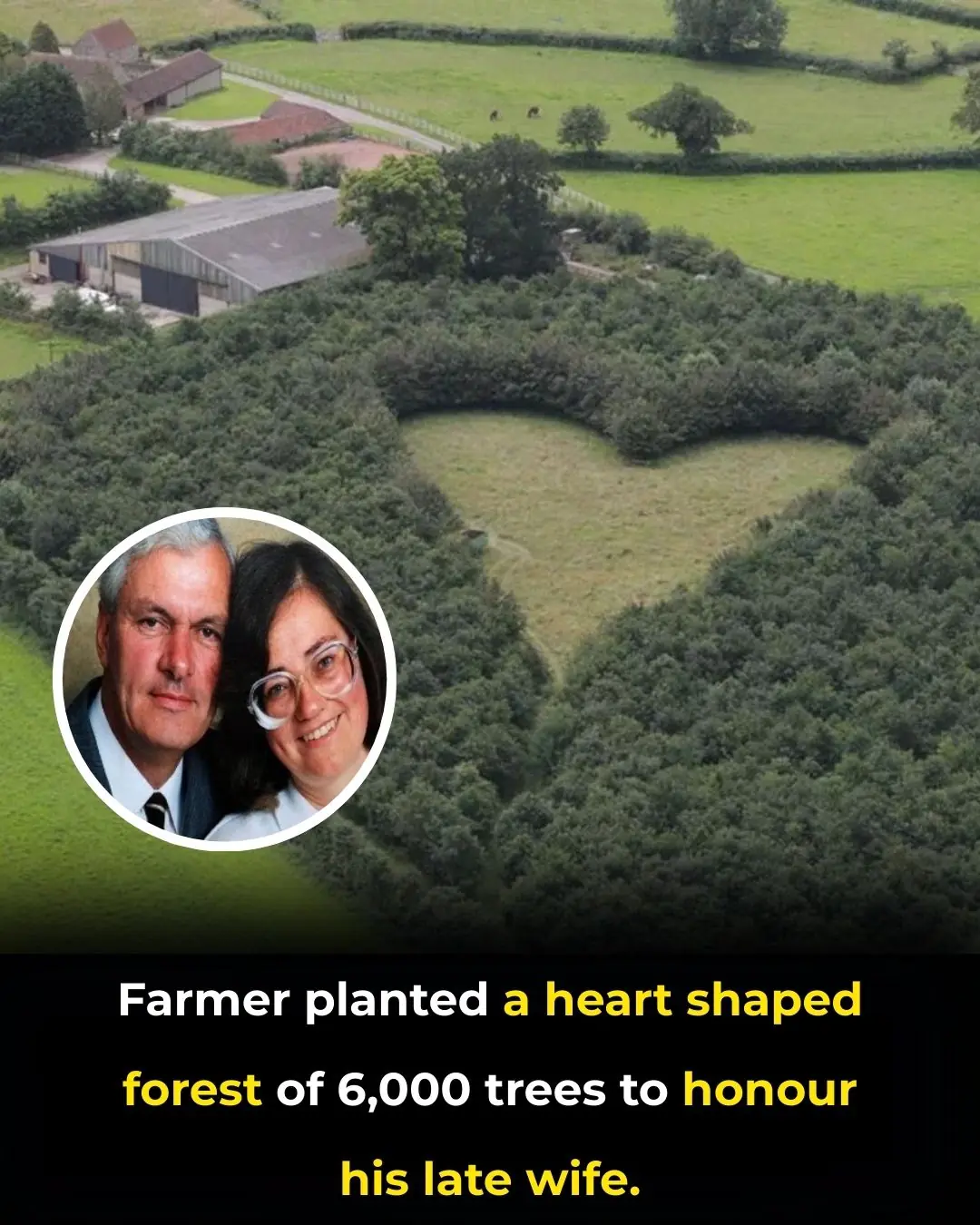
Planting Love That Endures: The Heart-Shaped Forest of Winston Howes