
There’s a Crusty Spot That Keeps Scabbing and Reopening — What Could It Be?
Noticing a small, crusty spot on your skin that repeatedly scabs over, heals slightly, and then reopens can be unsettling. When you can’t get in to see a healthcare provider right away, it’s natural to feel anxious and start wondering what it might mean. While many skin changes are harmless, a lesion that refuses to heal should never be ignored.
Understanding the most common causes of a persistent crusty spot — and knowing how to care for it safely while waiting for an appointment — can help you protect your skin and recognize when more urgent attention is needed. This article explores actinic keratosis, one of the most likely explanations, along with other possible causes, warning signs, and practical interim care steps recommended by dermatology experts.
1. Why a Recurrent, Crusty Spot Deserves Attention
Healthy skin typically heals within a few weeks. When a spot repeatedly scabs and reopens, it suggests that the underlying skin is not repairing itself properly. Dermatologists consider non-healing lesions a potential red flag, especially when they persist longer than four to six weeks.
Such spots may indicate chronic inflammation, sun damage, or early skin cancer changes. According to the American Academy of Dermatology (AAD), early evaluation of suspicious lesions greatly improves outcomes, particularly if the cause is precancerous or malignant (AAD, 2024).
2. Actinic Keratosis: A Common and Often Overlooked Cause
One of the most common causes of a recurring crusty patch is actinic keratosis (AK). These lesions develop after years of cumulative sun exposure and often appear on areas frequently exposed to ultraviolet (UV) radiation, such as the face, scalp, ears, neck, forearms, and hands.
Actinic keratoses are considered precancerous, meaning they are not cancer themselves but have the potential to progress into squamous cell carcinoma if left untreated. The Skin Cancer Foundation reports that up to 10% of untreated AKs may evolve into skin cancer over time, making early detection essential.
3. How Long-Term Sun Damage Leads to These Patches
UV radiation damages the DNA of skin cells, impairing their ability to grow and repair normally. Over time, this damage accumulates, especially in people with fair skin, light eyes, or a history of frequent sunburns.
The Mayo Clinic explains that actinic keratosis often reflects years of sun exposure rather than recent behavior. Even people who now practice good sun protection may develop AKs later in life due to past exposure.
4. What Actinic Keratosis Looks and Feels Like
In real life, actinic keratosis does not always look dramatic. It may present as:
-
A rough, dry, or scaly patch
-
Skin that feels like sandpaper
-
A red, pink, flesh-colored, or brown area
-
Mild itching, tenderness, or burning
Some people notice the texture before they see the spot clearly. Lesions are often small at first but can slowly enlarge or thicken.
5. When a Persistent Scab Could Mean Skin Cancer
Not every crusty spot is dangerous, but certain features raise concern. Both basal cell carcinoma and squamous cell carcinoma can appear as sores that bleed, crust over, and fail to heal.
According to the NHS and the AAD, warning signs include:
-
Bleeding without injury
-
Rapid growth or change in appearance
-
Pain, ulceration, or hardening
-
Irregular borders or uneven color
Any lesion with these features should be assessed as soon as possible.
6. Other Possible Causes Besides Actinic Keratosis
Several non-cancerous conditions can also cause recurring scabs:
-
Eczema, which can lead to inflamed, itchy patches that break and crust
-
Psoriasis, characterized by thick, scaly plaques
-
Contact dermatitis from allergens or irritants
-
Repeated friction, shaving irritation, or insect bites
These conditions are usually less dangerous but still benefit from proper diagnosis and treatment.
7. Why Viral Skin “Fixes” Can Make Things Worse
Social media is full of DIY skin remedies, but many can worsen a fragile lesion. Applying acidic substances like lemon juice, abrasive scrubs, or essential oils may damage the skin barrier and delay healing.
Dermatologists consistently warn against self-treating suspicious lesions with home remedies, as noted by the American Academy of Dermatology. Irritation can mask symptoms and complicate diagnosis later.
8. Safe At-Home Care While Waiting for an Appointment
If you can’t be seen right away, focus on protecting the area:
-
Gently cleanse with fragrance-free products
-
Apply a plain moisturizer or petrolatum jelly
-
Use broad-spectrum sunscreen (SPF 30+) daily
-
Avoid picking, scratching, or exfoliating the spot
These steps help reduce inflammation and prevent further damage without interfering with medical evaluation.
9. Red Flags That Require Urgent Medical Attention
Seek prompt care if the spot:
-
Bleeds repeatedly or spontaneously
-
Grows quickly or changes color
-
Becomes painful or infected
-
Is accompanied by fever or unexplained weight loss
These signs may indicate a more serious condition requiring immediate assessment.
10. How Dermatologists Diagnose and Treat Actinic Keratosis
Diagnosis is often made by visual examination, though a skin biopsy may be performed if cancer is suspected. Treatment options vary and may include:
-
Cryotherapy (freezing with liquid nitrogen)
-
Prescription topical medications
-
Photodynamic therapy
-
Minor surgical removal
Regular follow-ups are essential, as people with one AK are more likely to develop others.
11. Preventing Future Crusty Spots
Prevention centers on sun protection:
-
Daily sunscreen use, even in winter
-
Protective clothing and wide-brimmed hats
-
Avoiding tanning beds
-
Seeking shade during peak UV hours
These habits significantly reduce the risk of future lesions, according to the Skin Cancer Foundation.
12. Questions to Ask When You See a Doctor
When you’re finally seen, ask:
-
What is the most likely diagnosis?
-
Do I need a biopsy?
-
What treatment options are best for me?
-
How often should I have skin checks?
Understanding your condition empowers you to protect your skin long-term.
Trusted Sources
-
American Academy of Dermatology (AAD)
-
Mayo Clinic
-
NHS (UK)
-
Skin Cancer Foundation
News in the same category


Study Says That Crows Can Hold A Grudge For Up To 17 Years
What It Means If Your Fingers Turn White When It’s Cold
There are foods that go straight to the belly. Check comments 👇

Most Don’t Know: 12 Brilliant Ways to Use WD-40 Around the House (and What to Avoid)

My Nana Taught Me This Hack to Whiten Yellow Pillows in 5 Minutes With Zero Work — Here’s How It Actually Works
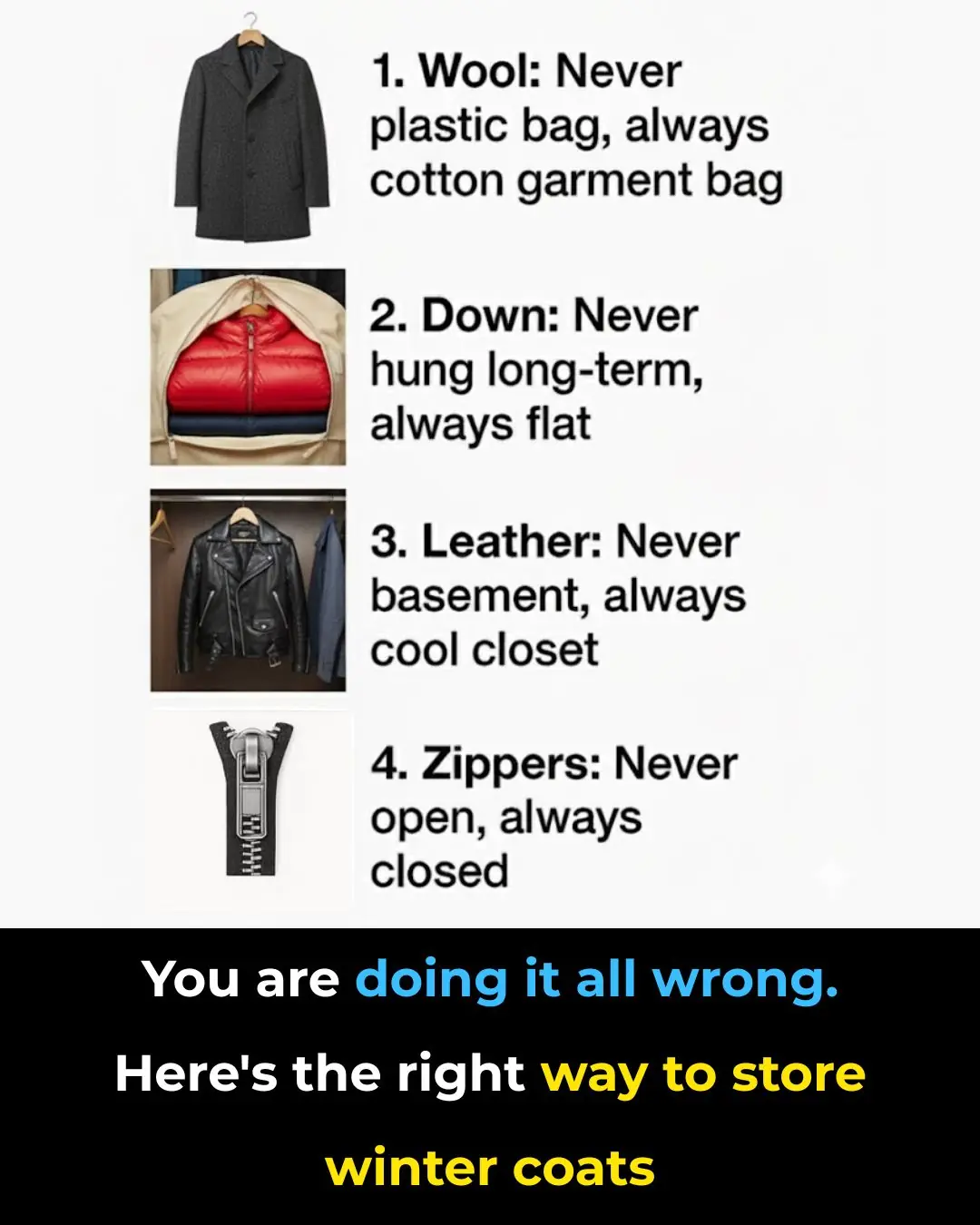
You’re Probably Storing Winter Coats All Wrong — Here’s the Right Way to Do It
Scientists Trigger Cancer Cells to Destroy Themselves From the Inside Out
A Chocolate Compound May Help the Brain Reclaim Its Youth
Your Outdoor Faucet Froze and Water Is Leaking Indoors — What to Do Immediately Before a Plumber Arrives

Why Christmas Cactus Buds Suddenly Fall Off — And What Usually Causes It

The Easy, Proven Way to Grow Lavender from Cuttings Most Gardeners Don’t Know

Everyone Has Made This Mistake When Using An Air Fryer
Your $2 Bill May Be Worth a Lot More Than You Think
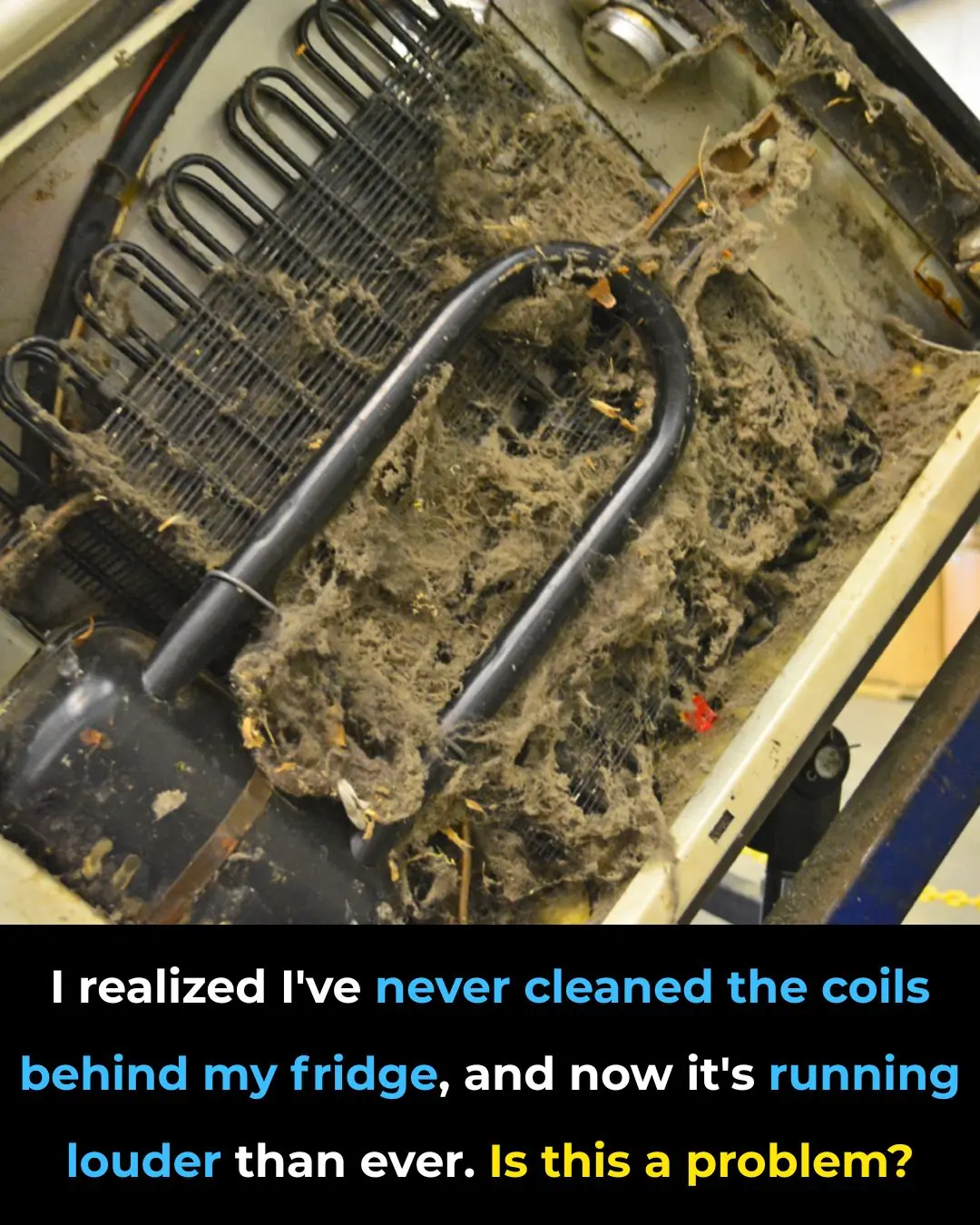
Is Your Refrigerator Too Loud? Why Dirty Condenser Coils Could Be the Reason—and What You Should Do

1 Lemon Is All It Takes to Revive a Struggling Orchid. Here’s Why It Works
My Nana’s 4-Minute Grill Hack Removes Burnt-On Gunk With Zero Scrubbing

10 Plants You Should NEVER Plant Near Lavender

I Had No Idea About This! One Simple Switch in Your Home That Can Lower Your Electricity Bill
News Post
Scientists Discover The Maximum Age a Human Can Live To
UC San Diego Health Performs World’s First Personalized Anterior Cervical Spine Surgery Using AI and 3D Printing

Tomato Benefits for Skin: Simple DIY Recipes for Glowing, Healthy Skin
Could Your Blood Type Be Influencing How You Age

Promising Early Results for ELI-002 2P: A New Vaccine Targeting Pancreatic Cancer

DIY Aloe Vera Oil for Hair Growth: Achieve Thick, Healthy Hair Naturally

Best Seeds for Hair Growth: Natural Remedies for Strong, Shiny Hair
Inflammation Is On Your Plate: 20 Foods That Harm Your Body And 20 That Heal
Create Your Own Hair Tonic: Add These Natural Ingredients to Your Hair Oil

Study Says That Crows Can Hold A Grudge For Up To 17 Years

Clove, Flaxseed, and Rose Water Toner: A Natural Alternative to Botox

Scientists Warn: Don’t Strip Moss Off Surfaces—It Absorbs Four Times More CO₂ Than Trees

Study Says That Crows Can Hold A Grudge For Up To 17 Years
The Hidden Power of Garlic: 7 Powerful Uses Beyond Cooking
Inflammation Is On Your Plate: 20 Foods That Harm Your Body And 20 That Heal

12 Signs You Have a Spiritual Gift (Even If You Don’t Realize It Yet)

Children Who Are Hugged Often Have Stronger Immune Systems, Studies Show

1 Cup to Cleanse Your Lungs of Phlegm and Toxins

Study Finds This Popular Sweetener Damages the Brain’s Protective Barrier
