Ulcerative Colitis vs. Crohn’s Disease: What Makes Them Different
Abdominal pain, chronic diarrhea, fatigue—these symptoms are often grouped under one name: Inflammatory Bowel Disease (IBD). But IBD actually includes two distinct conditions with important differences: Ulcerative Colitis and Crohn’s Disease.
Although they share overlapping symptoms, these diseases affect different parts of the digestive tract, behave differently over time, and require tailored treatment strategies. Understanding which one you’re dealing with can significantly improve long-term outcomes.
What Is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease is an umbrella term for chronic inflammatory disorders of the digestive tract caused by an abnormal immune response.
The two main types are:
-
Ulcerative Colitis
-
Crohn’s Disease
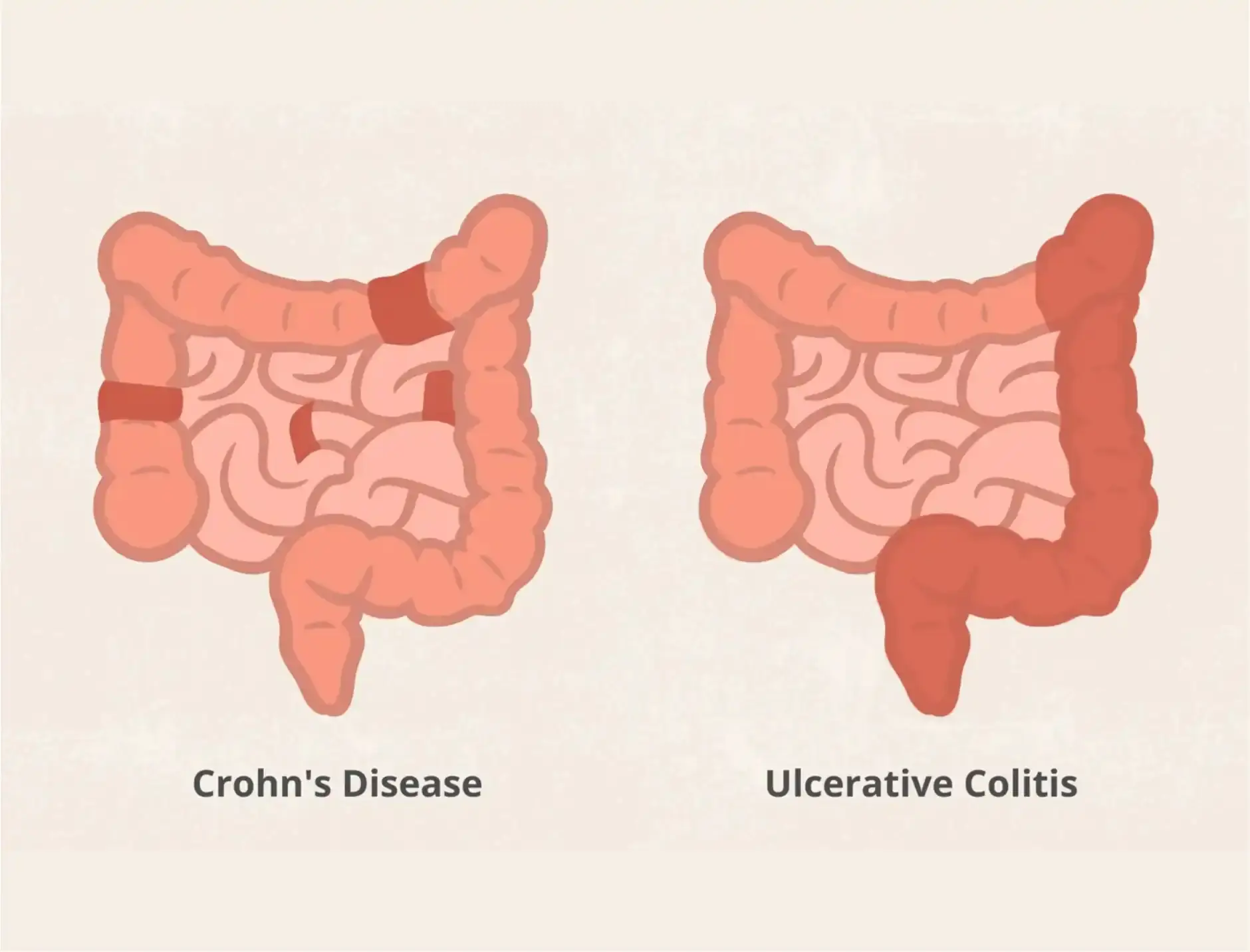
Ulcerative Colitis: Key Characteristics
Ulcerative colitis (UC) affects only the large intestine (colon and rectum) and causes continuous inflammation along the inner lining.
Where It Occurs
-
Starts in the rectum
-
Spreads upward through the colon
-
Never affects the small intestine
How It Damages the Gut
-
Inflammation is continuous
-
Affects only the mucosal (inner) layer
-
Leads to ulcers and bleeding
Common Symptoms
-
Bloody diarrhea
-
Urgent bowel movements
-
Rectal pain
-
Abdominal cramping
-
Fatigue and anemia
Crohn’s Disease: Key Characteristics
Crohn’s disease is more unpredictable and can affect any part of the digestive tract, from mouth to anus.
Where It Occurs
-
Most commonly the end of the small intestine (ileum)
-
Can skip healthy areas between inflamed sections (“skip lesions”)
How It Damages the Gut
-
Inflammation is patchy
-
Affects all layers of the bowel wall
-
Can cause fistulas, strictures, and abscesses
Common Symptoms
-
Chronic diarrhea (sometimes without blood)
-
Abdominal pain, often in the lower right abdomen
-
Weight loss
-
Malnutrition
-
Fever
Side-by-Side Comparison
| Feature | Ulcerative Colitis | Crohn’s Disease |
|---|---|---|
| Location | Colon & rectum only | Anywhere in GI tract |
| Pattern | Continuous inflammation | Patchy inflammation |
| Depth | Inner lining only | All bowel layers |
| Bloody stools | Common | Less common |
| Surgery outcome | Can be curative | Not curative |
Which Disease Is More Severe?
Neither condition is “better” or “worse”—they’re different.
-
UC carries a higher risk of colon cancer over time.
-
Crohn’s causes more structural complications like bowel obstruction.
-
Crohn’s is harder to treat surgically due to recurrence.
Severity depends on disease extent, flare frequency, and response to treatment.
Causes and Risk Factors (Both Conditions)
-
Genetic predisposition
-
Overactive immune response
-
Environmental triggers
-
Gut microbiome imbalance
-
Smoking (worsens Crohn’s, may reduce UC symptoms)
How Doctors Diagnose UC vs. Crohn’s
Diagnosis may include:
-
Colonoscopy with biopsy
-
Imaging (CT or MRI enterography)
-
Blood tests for inflammation
-
Stool markers (calprotectin)
Accurate diagnosis is critical—treatments are not interchangeable.
Treatment Approaches
Shared Treatments
-
Anti-inflammatory drugs (5-ASA)
-
Corticosteroids for flares
-
Immunosuppressants
-
Biologic therapies
Surgery Differences
-
Ulcerative colitis: Removing the colon can cure the disease
-
Crohn’s disease: Surgery treats complications but disease often returns
Diet and Lifestyle Support
While diet doesn’t cause IBD, it strongly affects symptoms.
Helpful strategies:
-
Smaller, frequent meals
-
Low-residue diet during flares
-
Avoid trigger foods (fatty, spicy, dairy if sensitive)
-
Stress management and adequate sleep
When to See a Doctor Urgently
-
Persistent bloody stools
-
Severe abdominal pain
-
Unexplained weight loss
-
Fever with digestive symptoms
-
Signs of dehydration or anemia
Early treatment can prevent irreversible bowel damage.
Final Thoughts
Ulcerative colitis and Crohn’s disease may look similar on the surface—but their behavior, risks, and management are very different. A precise diagnosis empowers better decisions, fewer complications, and a higher quality of life.
If your symptoms don’t fit neatly into one category, keep asking questions. In IBD, clarity is power.
News in the same category

12 Bizarre Symptoms of Vitamin D Deficiency You Need to Know

8 warning signs of colon cancer you should never ignore

The daily drink that helps clear blocked arteries naturally

This old school home remedy will soothe your back, joints & knee pain in just 7 days!

Sleep Apnea: Symptoms, Risks, and Treatment Solutions
Viral Pneumonia vs. Bacterial Pneumonia: Key Differences

Allergic Rhinitis: What Triggers It and How to Manage It
COPD Exacerbation: Symptoms That Indicate a Flare-Up
Bile Reflux vs. Acid Reflux: Key Differences You Need to Know
How to lower blood sugar without giving up carbs

Top 8 warning signs of ovarian cancer women absolutely need to know
Don’t Ignore These Warning Signs of Vitamin B12 Deficiency!
Why you keep waking up with dry mouth—and what it may be telling you

Here’s What Eating Blueberries Every Day Does to Your Body, Says a Registered Dietitian
How To Get Rid Of Eczema: 13 Natural Remedies Backed By Research
Scientists Explain The Effects of Eating Too Much Sugar

Top 10 Functional Foods In The World Which Fight Cancer Cells
90% of diabetes cases could end if you STOP these foods
News Post
The Meaning of Having an Unmade Bed
Put a few ice cubes in the washing machine with your wrinkled clothes and do this, and you'll see an unexpected miracle.
A 2013 study conducted by researchers

Experienced tofu makers share tips on how to distinguish between clean tofu and tofu containing gypsum.

Don't put the purchased sấu fruit in the refrigerator right away: Follow this one extra step, and the sấu fruit will stay fresh and delicious for a whole year, retaining its original flavor.

How Retired Buses in France Are Becoming Mobile Book Rooms for Thoughtful Travel

How Turkey’s ‘Micro Animal Closets’ Are Offering Care to Stray Animals in Urban Parks

How Portugal Is Turning Urban Parking Towers into Night Shelters for the Homeless

How Retroftted City Buses Are Providing Warmth and Rest for the Homeless in Canada

People with heart problems should avoid these 4 things to reduce stimulation to the heart
12 Bizarre Symptoms of Vitamin D Deficiency You Need to Know

8 warning signs of colon cancer you should never ignore

The daily drink that helps clear blocked arteries naturally

This old school home remedy will soothe your back, joints & knee pain in just 7 days!

Sleep Apnea: Symptoms, Risks, and Treatment Solutions
Always the Strong One: The Emotional Cost of Holding Everything Together

A New Cancer Vaccine Shows Long-Lasting Protection in Preclinical Studies
Viral Pneumonia vs. Bacterial Pneumonia: Key Differences

Allergic Rhinitis: What Triggers It and How to Manage It